Surgical Management of Total Proctocolectomy with Ileal J-Pouch Anal Reconstruction for Severe Ulcerative Colitis: Rare Case Report
Joko Wibowo Sentoso* and Suryo Wahyu Raharjo
Published Date: 2025-03-20Joko Wibowo Sentoso*, Suryo Wahyu Raharjo
Department of Surgery, Faculty of Medicine, Sebelas Maret University/Dr. Moewardi Hospital, Surakarta, Indonesia
- *Corresponding Author:
- Joko Wibowo Sentoso
Department of Surgery,
Faculty of Medicine, Sebelas Maret University/Dr. Moewardi Hospital, Surakarta,
Indonesia
E-mail: jokowibowo.dr@gmail.com
Received date: April 20, 2024, Manuscript No. IPDD-24-18901; Editor assigned date: April 23, 2024, PreQC No. IPDD-24-18901 (PQ); Reviewed date: May 07, 2024, QC No. IPDD-24-18901; Revised date: March 13, 2025, Manuscript No. IPDD-24-18901 (R); Published date: March 20, 2025, DOI: 10.36648/IPDD.11.1.54
Citation: Sentoso JW, Raharjo SW (2025) Surgical Management of Total Proctocolectomy with Ileal J-Pouch Anal Reconstruction for Severe Ulcerative Colitis: Rare Case Report. G J Dig Dis Vol:11 No:1.
Abstract
Introduction: Ulcerative colitis is a chronic, relapsing, and potentially progressive form of Inflammatory Bowel Disease (IBD) characterized by inflammation localized to the mucosa of the rectum and colon. The etiology of ulcerative colitis is uncertain, several of etiological factors such as genetic predisposition, disturbances in the gut microbiome, immune dysregulation and environmental triggers have been implicated. There has been an evolution in the treatment of ulcerative colitis since the 1950's. From conventional management it evolved to the use of broadspectrum anti-inflammatory drugs such as amino-salicylates and corticosteroids, or immunomodulators, such as thiopurines, often sequentially. This therapy aims to relieve symptoms and achieve remission to prevent long-term complications.
Case presentation: A 69-years old woman complained of continuous diarrhea for 2 months. Complaints accompanied by malaise, nausea, mild fever and weight loss of 5 kg. The abdominal examination was performed, there was pain over the entire surface of the stomach which was not typical, there was no distension, bowel sounds were within normal limits, and percussion pads were found tympanic sound. The patient had a history of a colonoscopy and biopsy performed in March 2024. The patient was decided to receive Total proctocolectomy surgical therapy with ileal Jpouch anal reconstruction and ileostomy.
Discussion: Ileal-Pouch-Anal Anastomosis (IPAA) is a standard therapeutic procedure that is part of total proctocolectomy for ulcerative colitis patients. A systematic review study showed that the risk of high-grade dysplasia was quite low at 0.15% after restorative proctocolectomy and the frequency was similar in the pouch, anal transition zone and rectal cuff. With the use of stapled anastomosis, the length of the rectal cuff is one of the main determinants of quality of life after surgery. In this case the patient was diagnosed with severe ulcerative colitis. The diagnosis is made through history taking, physical examination, laboratory examination and colonoscopy with biopsy. Total proctocolectomy surgical therapy with ileal J-pouch anal reconstruction and ileostomy was perform, even though that procedure had complications such as abscesses, sepsis, fistulas and impaired fertility and sexual function postsurgery. The procedure was still carried out considering the severity of the disease.
Conclusion: We recommend total proctocolectomy with ileal J-pouch anal reconstruction as an alternative procedure that is safe, feasible, effective, and has a relatively low postoperative complication rate for patients with severe ulcerative colitis.
Keywords
Severe ulcerative colitis, Total proctocolectomy, Ileal j-pouch anal reconstructio
Introduction
Ulcerative colitis is a chronic, relapsing, and potentially progressive form of Inflammatory Bowel Disease (IBD) characterized by inflammation localized to the mucosa of the rectum and colon. The etiology of ulcerative colitis is uncertain, several of etiological factors such as genetic predisposition, disturbances in the gut microbiome, immune dysregulation and environmental triggers have been implicated. There has been an evolution in the treatment of ulcerative colitis since the 1950's. From conventional management it evolved to the use of broad-spectrum anti-inflammatory drugs such as amino-salicylates and corticosteroids, or immunomodulators, such as thiopurines, often sequentially. This therapy aims to relieve symptoms and achieve remission to prevent long-term complications [1].
The main symptoms of ulcerative colitis include bloody diarrhea, with or without mucus, tenesmus, abdominal pain, malaise, weight loss, and fever, depending on the extent and severity of the disease. The onset of the disease is usually gradual, and patients will likely experience periods of spontaneous remission and then relapse [2]. The diagnosis of ulcerative colitis can be made clinically with supportive findings on negative stool examination, endoscopy, biopsy aimed at determining the cause of infection. As colonic infections can produce clinical findings that are indistinguishable from idiopathic ulcerative colitis, microbiological studies for bacterial infection and parasitic infestation should be included in the initial diagnostic evaluation [3,4].
The radiological examination in this case is not particularly recommended for diagnosis but may be useful. Patients with long-standing ulcerative colitis may show a “stove pipe” appearance on Double Contrast Barium Enema (DCBE) examination. Colonoscopy or proctosigmoidoscopy can also be used as a diagnostic tool demonstrating loss of the characteristic vascular pattern, granularity, friability, and ulceration, involving the distal rectum and progressing proximally in a symmetrical, continuous, and circular pattern. This disorder can occur locally in the rectum and sigmoid colon (proctitis) to include the entire large intestine (pancolitis). Population-based studies show that, based on symptoms, proctitis is found in 30-60% of patients, left-sided colitis is found in 16-45%, and pancolitis is found in 14-35%. Laboratory examination usually shows an increase in inflammatory factors such as ESR, CRP, leukocytosis, especially in acute attacks. Regardless of the stage of the disease, 60-70% of ulcerative colitis patients are positive for Perinuclear Antineutrophil Cytoplasmic Antibodies (P-ANCA) which are found in a small number of Crohn's disease patients. Anti-Saccharomyces Cerevisiae Antibodies (ASCA) are also found in Crohn's disease and ulcerative colitis but are more common in Crohn's disease. Therefore, testing for P-ANCA and ASCA has utility in differentiating ulcerative colitis and Crohn's disease. Carcinoembryonic Antigen (CEA) testing can also be helpful in ulcerative colitis, usually higher levels can indicate a recurrence of the disease.
Emergency indications for surgery include refractory toxic megacolon, perforation, and persistent severe colorectal bleeding [5,6]. In this situation, the recommended operations include colectomy and ileostomy, as well as preserving the segment of distal rectum in place, because reconstruction is not an option in acute conditions. Elective surgery is indicated in chronic chronic colitis refractory to immunosuppressive treatment, detection of dysplasia or malignancy, and luminal narrowing diseases causing partial or complete intestinal obstruction. The recommended surgery is total proctocolectomy with Ileal-Pouch-Anal Anastomosis (IPAA). Although with IPAA curative therapy for Ulcerative Colitis is available, IPAA has a high rate of postoperative complications, reaching 20% with abscesses, sepsis, fistulas, and impaired fertility and sexual function post-surgery [7-9]. Ileorectal anastomosis is a temporary alternative in certain cases (for example in young women who have not had children), but carries the risk of disease recurrence and/or the development of cancer in the remaining rectal segment.
Case Presentation
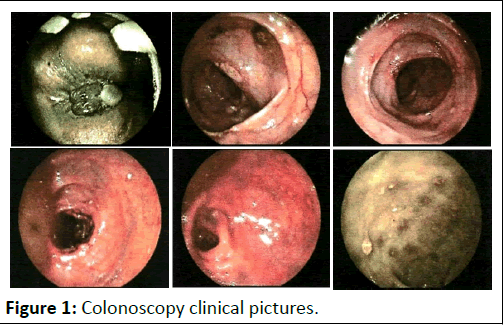
A 69-years old woman complained of continuous diarrhea for 2 months. Complaints accompanied by malaise, nausea, mild fever and weight loss of 5 kg. The patient's vital signs showed blood pressure 143/76 mmHg, heart rate 78 times/minute, respiratory rate 18 times/minute, temperature 36.6°C. The patient's body mass index was included in the underweight category (20.88 kg/m2, body weight: 52 kg; TB: 158 cm). The abdominal examination was performed, there was pain over the entire surface of the stomach which was not typical, there was no distension, bowel sounds were within normal limits, and percussion were found tympanic sound. The chest and extremities examination were no abnormalities. The patient had a history of a colonoscopy and biopsy performed in March 2024, and the results were ulcerative colitis in the colon and rectosigmoid (Figure 1).
Figure 1: Colonoscopy clinical pictures.
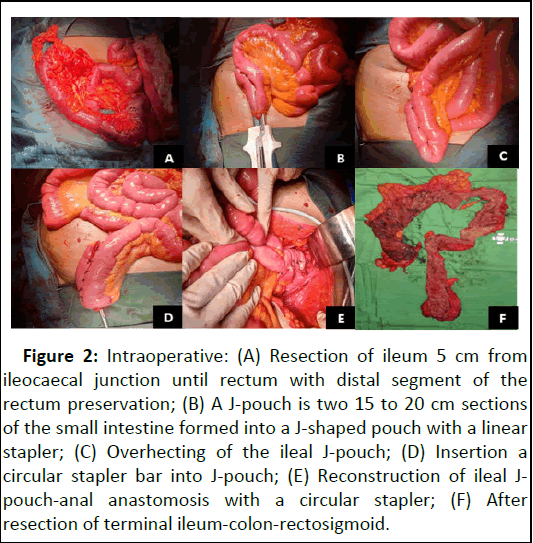
Hematologic assessment in March 2024 showed that hemoglobin concentration was 12.4 g/L; mean cell volume was 37 fL, white blood cell counts was 7.6 g/L, platelet count 585 g/L. Biochemical assessment based on urea 17 mmol/L, creatinin 0.5 µmol/L. In this patient, P-ANCA, ASCA, and CEA were not checked. The patient was decided to receive total proctocolectomy surgical therapy with ileal J-pouch anal reconstruction and ileostomy, the clinical pictures of during operation can be seen in Figure 2.
Figure 2: Intraoperative: (A): Resection of ileum 5 cm from ileocaecal junction until rectum with distal segment of the rectum preservation; (B): A J-pouch is two 15 to 20 cm sections of the small intestine formed into a J-shaped pouch with a linear stapler; (C): Overhecting of the ileal J-pouch; (D): Insertion a circular stapler bar into J-pouch; (E): Reconstruction of ileal J-pouch-anal anastomosis with a circular stapler; (F): After resection of terminal ileum-colon-rectosigmoid.
After surgical procedure, the patient received post-operative treatments including Totilac infusion 1500 cc/24 hours, Ampicillin/Sulbactam injection 1.5 gr/8 hours, Metamizole injection 1 gr/8 hours. After surgery, the patient was treated for 5 days. Then the patient was outward and advised to go to the digestive surgery clinic for evaluation.
Discussion
Ileal-Pouch-Anal Anastomosis (IPAA) is a standard therapeutic procedure that is part of total proctocolectomy for Ulcerative Colitis (UC) patients. This technique has been developing since 1978 and was described by Sir Alan Parks and J. Nicholls [10]. There are several designs of such procedural bags, but the J bag allows shorter operating times with equally good long-term results [11]. The feasibility and safety of colectomy and pouch reconstruction procedures with IPAA have been clearly demonstrated by data published in 2011 and showing a relatively low complication rate after surgery [12]. The anastomosis can be double clamped, requiring preservation of the distal segment of the rectum, or mucosectomy and hand-sewn anastomosis can be performed, so that the affected rectal mucosa can be removed completely. The latter option shows worse continence and lower anal resting pressure [13]. A systematic review study showed that the risk of high-grade dysplasia was quite low at 0.15% after restorative proctocolectomy and the frequency was similar in the pouch, anal transition zone and rectal cuff [14]. Stapled IPAA is currently considered the standard procedure [15]. Mucosectomy and hand-sewn pouch-anal anastomosis are mostly performed in failed staple anastomoses presenting in less than 5% of procedures, although there is no clear evidence against their use [16]. With the use of stapled anastomosis, the length of the rectal cuff is one of the main determinants of quality of life after surgery. Cuff length >2 cm is associated with recurrence of inflammatory disease symptoms or neoplastic risk.
In this case the patient was diagnosed with severe ulcerative colitis. The diagnosis is made through history taking, physical examination, laboratory examination and colonoscopy with biopsy. Total proctocolectomy surgical therapy with ileal J-pouch anal reconstruction and ileostomy was perform, even though that procedure had complications such as abscesses, sepsis, fistulas and impaired fertility and sexual function post-surgery. The procedure was still carried out considering the severity of the disease.
Conclusion
We recommend total proctocolectomy with ileal J-pouch anal reconstruction as an alternative procedure that is safe, feasible, effective, and has a relatively low post-operative complication rate for patients with severe ulcerative colitis. The author's hope is that with this procedure patient can achieve a better quality of life. Hopefully, there will be case report or research regarding more complex cases and more advanced therapy modifications.
References
- Aslam N, Lo SW, Sikafi R, Barnes T, Segal J, et al. (2022) A review of the therapeutic management of ulcerative colitis. Therap Adv Gastroenterol 15
[Crossref] [Google Scholar] [PubMed]
- Lynch WD, Hsu R (2023) Ulcerative Colitis. Treasure Island (FL): StatPearls Publishing
- Gomollón F, Rubio S, Charro M, Garcia-Lopez S, Munoz F, et al. (2014) Reccomendations of the Spanish Working Group on Crohn's Disease and Ulcerative Colitis (GETECCU) on the use of methotrexate in inflammatory bowel disease. Gastroenterol Hepatol 38:24-30
[Crossref] [Google Scholar] [PubMed]
- Lee JS, Kim ES, Moon W (2019) Chronological review of endoscopic indices in inflammatory bowel disease. Clin Endosc 52:129-136
[Crossref] [Google Scholar] [PubMed]
- Berg DF, Bahadursingh AM, Kaminski DL, Longo WE (2002) Acute surgical emergencies in inflammatory bowel disease. Am J Surg 184:45-51
[Crossref] [Google Scholar] [PubMed]
- Andersson P, Söderholm JD (2009) Surgery in ulcerative colitis: Indication and timing. Dig Dis 27:335-340
[Crossref] [Google Scholar] [PubMed]
- Loftus Jr EV, Delgado DJ, Friedman HS, Sandborn WJ (2008) Colectomy and the incidence of postsurgical complications among ulcerative colitis patients with private health insurance in the United States. Am J Gastroenterol 103:1737-1745
[Crossref] [Google Scholar] [PubMed]
- Waljee A, Waljee J, Morris AM, Higgins PD (2006) Threefold increased risk of infertility: A meta-analysis of infertility after ileal pouch anal anastomosis in ulcerative colitis. Gut 55:1575-1580
[Crossref] [Google Scholar] [PubMed]
- Hueting WE, Buskens E, van der Tweel I, Gooszen HG, van Laarhoven CJ (2005) Results and complications after ileal pouch anal anastomosis: A meta-analysis of 43 observational studies comprising 9,317 patients. Dig Surg 22:69-79
[Crossref] [Google Scholar] [PubMed]
- Capolupo GT, Carannante F, Mascianà G, Lauricella S, Mazzotta E, et al. (2021) Transanal proctocolectomy and Ileal Pouch-Anal Anastomosis (TaIPAA) for ulcerative colitis: Medium term functional outcomes in a single centre. BMC Surg 21:1-7
[Crossref] [Google Scholar] [PubMed]
- McCormick PH, Guest GD, Clark AJ, Petersen D, Clark DA, et al. (2012) The ideal ileal-pouch design: A long-term randomized control trial of J-vs W-pouch construction. Dis Colon Rectum 55:1251-1257
[Crossref] [Google Scholar] [PubMed]
- Fleming FJ, Francone TD, Kim MJ, Gunzler D, Messing S, et al. (2011) A laparoscopic approach does reduce short-term complications in patients undergoing ileal pouch-anal anastomosis. Dis Colon Rectum 54:176-182
[Crossref] [Google Scholar] [PubMed]
- Schluender SJ, Mei L, Yang H, Fleshner PR (2006) Can a meta-analysis answer the question: Is mucosectomy and handsewn or double-stapled anastomosis better in ileal pouch-anal anastomosis?. Am Surg 72:912-916
[Crossref] [Google Scholar] [PubMed]
- Scarpa M, van Koperen PJ, Ubbink DT, Hommes DW, Kate FJT, et al. (2007) Systematic review of dysplasia after restorative proctocolectomy for ulcerative colitis. Br J Surg 94:534-545
[Crossref] [Google Scholar] [PubMed]
- Lovegrove RE, Tilney HS, Remzi FH, Nicholls RJ, Fazio VW, et al. (2011) To divert or not to divert: A retrospective analysis of variables that influence ileostomy omission in ileal pouch surgery. Arch Surg 146:82-88
[Crossref] [Google Scholar] [PubMed]
- Øresland T, Bemelman WA, Sampietro GM, Spinelli A, Windsor A, et al. (2015) European evidence based consensus on surgery for ulcerative colitis. J Crohns Colitis 9:4-25
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences