Levels in Decision Making and Techniques for Clinicians
Michele Molinari, Sanem Guler,Scott Hurton,Matt C winn,
DOI10.4172/2472-1891.100002
Sanem Guler, Scott Hurton, Matt C winn and Michele Molinari*
Department of Surgery, Dalhousie University, Queen Elizabeth II Health Sciences Centre, Halifax, Nova Scotia, Canada.
- *Corresponding Author:
- Michele Molinari
Associate Professor, Department of Surgery
Room 6-302 Victoria Building 1276 South Park Street Halifax, Canada B3H 2Y9
Tel: +1-902-473-7624
Fax: 91-821-2517233
E-mail: Michele.molinari@cdha.nshealth.ca
Citation: Michele Molinari, et al. Levels in Decision Making and Techniques for Clinicians. Int J Dig Dis. 2015, 1:1. doi:10.4172/2472-1891.100002
Abstract
In the last century, there has been tremendous advancements in medicine and surgery and this progress has resulted in an over expansion of the number of treatment options that are available to treat many conditions. The enlarging armamentarium available to modern physicians should be celebrated. However, this has come with a significant increase in the complexity of decisions that physicians have to make when they select a therapy among many that have comparable efficacy. For example, small hepatocellular carcinomas can be treated with liver transplantation, surgical resection or locoregional therapies, with similar overall survival but different disease free survival and morbidities. One of the primary goals of decision analysis is to help decision makers. In healthcare, this translates in more cost-effective treatments, higher patients’ satisfaction and overall better outcomes. Because judgments of uncertainty are a critical part of medical decision-making, decision analysis tends to improve the accuracy of these judgments by using specific algorithms and techniques. The main aim of this review is to make clinicians familiar with the different levels of decision analysis. In this paper, we will describe common techniques that are used to elicit patients’ preferences, the meaning of utilities and the benefit and limitations of decision analysis in health care.
Introduction
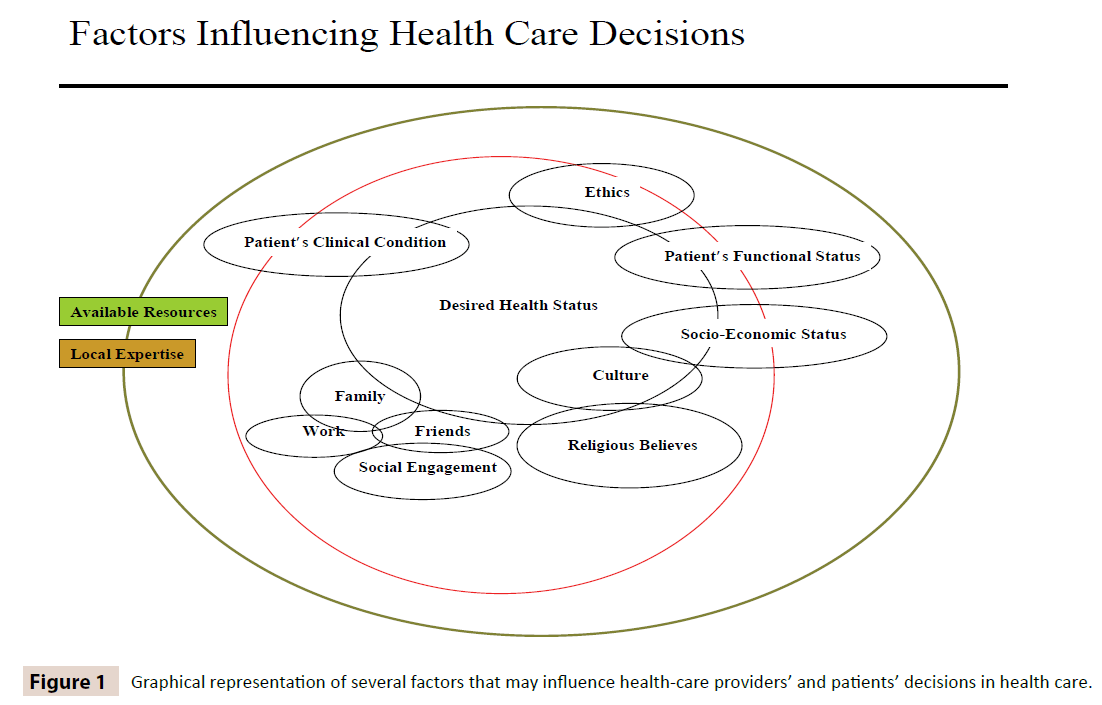
In recent years, the patients’ rights movement has sought to increase involvement of patients in decisions about their care since their active participation improves their outcomes [1-6]. This might be due to better compliance or to the overall benefits that come when patients are engaged and actively looking for their full recovery. When physicians elicit patients’ preferences for an intervention (medical therapy or surgical procedure), they have an opportunity to explain what are the potential risks and benefits of all the available treatment options. Therefore, in 2007, a new legislation in the United States has officially recognized that shared decisions, between caregivers and patients, is necessary and represents the highest standard of informed consent [7]. However, to reach the ambitious goal of incorporating patients’ views and values using shared decision methods, physicians and other caregivers need to be familiar with decision analysis techniques [8-13].. The vast majority of practicing clinicians already evaluate patients’ desires and their expectations, but most of the times this is done in an implicit manner because health care decisions are often ethically difficult and time consuming as they need to take into account complex dimensions such as personal beliefs, faith, societal values, cultural, and socioeconomic pressures (Figure 1).
In healthcare, there are many situations where the most desirable decision depends entirely on how patients value the expected outcomes, and the relevant health states they will experience during and after their care is completed. For example, when dealing with patients with malignant diseases, the decision to choose longer survival versus side effects of the treatment should depend largely on what patients value the most. For all these reasons, decision analysis instruments that can be used at the bedside cannot only help patients, but also physicians who face difficult decisions. This review aims at illustrating the different levels and most common instruments used in decisionmaking. Since the discipline of decision-analysis is not mandatory during the formation of health-care providers, we hope that his review might be of some help to clinicians who are interested in exploring further this discipline.
Why is patients’ participation important?
Several studies have documented that in the adult population admitted to the hospitals for serious illnesses, caregivers do not have the time or resources to elicit patients’ preferences about the level of care they would like to receive in case of deterioration of their conditions [14-16]. There is some evidence that have shown that patients’ desire to be involved in making decisions related to their treatments depends on the nature of the perceived effects of these decisions (e.g. minor versus major), the nature of their illness (e.g. chronic versus acute) and the disease severity [17]. For example, when patients were asked to rank their inclinations towards being actively involved in their health care, patients expressed the desire to make major decisions with their physicians but preferred less involvement for minor issues [17]. On the other hand, other studies have shown that if the type of illness was more severe, patients’ desire for participation declined [18,19]. From current data, it seems that patients’ choice to play an active role in making decisions for their health depends on variables that are difficult to measure each time and for each patient. Therefore, DA has historically been used mostly for research purposes. Nevertheless, this should not remain the case as eliciting patients’ preferences often results in selecting therapies that are in line with their preferences and improve their compliance and their outcomes [20-23].
Evidence-Based Medicine and Clinical Decision Making
The value of any decision depends largely on the accuracy and validity of the information on which it is based [24]. Over the past decades, increasing attention has been paid to the scientific quality of research that provides the evidence used to support clinical practices [25] and to improve the process of decision-making [25]. The term evidence-based medicine refers to the application of evidence of the highest possible quality to clinical practice. In real life, a specific treatment might be selected because of a clinical trial showed superior results. Yet, the outcomes of any patient treated similarly to the individuals enrolled in that trial might deviate significantly from the overall results of the trial due to chance or other factors that might not be clearly identifiable.
Every practicing clinician is familiar with the concept that outcomes mainly depend on what therapeutic choices are made after the correct diagnosis is made. However, even if the treatment is correct, the final outcomes cannot be known with certainty at the moment of the decision [26]. Because judgments of uncertainty are a critical part of medical decision making, by using specific algorithms, decision analysis tend to improve the accuracy of these judgments.
Components of Clinical Decisions
Several factors play a role in clinical decisions. Among them, the most significant are:
1. The likelihood of accurate diagnosis in the face of less than perfect tests,
2. The likelihood of positive response to the therapy and
3. The likelihood of experiencing adverse events due to the intervention
When practicing evidence-based medicine, decisions preferentially rely on data from clinical trials if available. However, this process becomes less meaningful when data of trials are inadequate or applied to patients who deviate from the study population, when desired outcomes differ from those evaluated in the trials, or when the scope of diagnostic and therapeutic alternatives differ from those of the trials [27]. Therefore, in many circumstances, clinical decisions have to be made in the absence of good quality evidence that one treatment modality is better than others. In these circumstances, physicians usually base their decisions on observational studies, personal experience or case reports. Most of the times, they do not use decision analysis methods as the majority of clinicians are not very familiar with this methodology that can offer a complementary approach to evidence-based medicine by providing a logical and analytical method of identifying the key elements of uncertainty and strategies that might be able to optimize the desired outcomes [28]. For example, in a recent study by Cillo et al, [29]. the authors used a Markov model to assess the cost-utility of treating advanced intra-hepatic cholangiocarcinomas. In this study, three clinical scenarios were analyzed: the first was about patients with single intra-hepatic cholangiocarcinoma measuring more than 6 cm in diameter, the second was about patients with cholangiocarcinomas invading vascular structures and the third was about patients with multi-focal cholangiocarcinomas. The main aim of this study was to estimate the cost-effectiveness of uprfront hepatic resection with positive resection margins versus the use of neoadjuvant chemotherapy followed by possible curative hepatic resection. Since there were no randomized clinical trials that could help them to decide which strategy was the best one, the mathematical model helped them to recognize that patients with large intrahepatic cholangiocarcinomas, or with tumors invading vascular structures, upfront hepatic resection was more cost-effective than using neoadjuvant chemotherapy followed by surgery. This example is just one of many that can illustrate how decision analysis methods can assist clinicians and policy makers when dealing with difficult decisions where the degree of uncertainty is quite significant. However, it is important to keep in mind that there are many levels of decision-making in health care and that each level requires different methodologies.
Level of Decision Making In Health Care
There are four main levels of decision-making in the delivery of health care [30,31]. These four levels require different instruments that are summarized in (Table 1).
| Level of Decision Making | Measurement | Instrument used |
|---|---|---|
| Meta Level | Choices are made between various fields of public expenditure, e.g. health care versus defense or education. | Political decisions Macro-economic analysis |
| Macro Level | Preferences for allocation and utilization of resources. This level uses instruments that allow policy-makers to allocate funds for different health-care programs without considering the implications for individual patients. | Standard gamble Time trade-off Quality of Well-Being Scale Health Utility Index EuroQoL Rosser and Kind Index Person trade-off |
| Meso Level | Optimal treatment policy for groups of patients with similar clinical characteristics. This level uses instruments that allow clinicians to select treatments that have been shown to provide the best overall outcome for groups of patients affected by the same disease. At this level, individual’s preferences are not integrated in the decision making process. | Utilities Standard Gamble Time trade-off Visual analog scale |
| Micro Level | Patient’s own preferences. This level uses instruments that allow clinicians to select among several potential treatments to match patients’ expectations. The micro level aims at capturing individual’s preferences for competing therapeutic strategies. | Probability trade-off Magnitude estimation Person trade-off Willingness to pay Visual analogue scale Time trade-off Conjoint analysis |
Table 1: Summary of Levels of Decision-making in Health Care and the Instruments Used to Measure Utilities or Patients’ Preferences.
| Method | Characteristics | Limitations |
|---|---|---|
| Standard Gamble (SG) | Considered the gold standard to elicit utilities in health care as it incorporates trade-off risks. It has the highest level of content validity when risk is involved in the decision-making. | For some individuals it is difficult to understand, as it requires a comparison of probabilities. Method not sufficiently reliable for individual patient decision-making. |
| Time Trade Off (TTO) | It presents a task that is simpler to be understood than SG. As it deals with time, it is very convenient when making decisions about treatments where survival is the main issue. It has the highest level of content validity when the trade-off is between quality of life and length of life. | TTO requires that the respondents perform the task of trading off time rather than events. It requires the assumption that there is a constant proportional trade-off when dealing with future years of life. |
| Rating Scales (Visual Analog Scale VAS) | Ratings are performed on a scale that is conventionally anchored by best possible health (equal to 1) and worst possible health or death (equal to 0). | It does not measure utilities, as ratings do not incorporate any trade-off. Scales are not proportional. |
| Person Trade Off | Method that directly seeks information required for policy makers. It measures the societal worth of alternative health care interventions. It asks respondents to trade a lesser health benefit for a larger number of people against a larger benefit for a smaller number of people. | It does not measure utilities, as it does not incorporate any trade-off. Method not sufficiently reliable for individual patient decision-making. |
| Willingness to Pay (WTP) | Method developed in the context of cost-benefit analysis where health benefits are valued in monetary terms. It uses survey methods to elicit dollar values for nonmarket commodities such as health. | It does not measure utilities, as it does not incorporate any trade-off. Limited research is available where WTP is compared with other measures of health state preferences. Method not sufficiently reliable for individual patient decision-making. |
| Probability Trade Off (PTO) Conjoint Analysis (CA) | They allow researchers to elicit patients’ preferences among competing treatments. They can be used at the bedside and it can help patients to clarify and communicate their values. | They do not measure utilities. The resulting preference scores are specific to the original decision problem and only the strength of the preference for a treatment versus other competing alternatives is measured. |
Table 2: Summary of the most common decision analysis methods used to elicit health utilities or treatment preferences.
Meta Level
At this level, politicians and managers make decisions regarding the health care of large populations balancing the financial and humanitarian aspects of service delivery. For example, in countries where health-care is public, politicians need to decide what percentage of the total revenue will be delivered for health-care among all the other competing needs, e.g. education, defense, infrastructures, research etc. In addition, health ministers have to decide which programs to support and which ones to cut after careful consideration of the available budgets. For the majority, decisions at the meta-level are supported by data provided by computerized models or meta-data since the use of public resources should be based on the principle of maximizing the level of health for the majority of the population [32]. However, in many circumstances, decisions can be influenced by other forces and there have been no studies on how administrators and politicians make their decisions and what strategies they use when they need to address ethical issues arising from resource allocation [33].
Macro Level
The second level is also known as macro level. It concerns decisions on allocation and utilization of resources in a region, organization, hospital, etc. Because resources dedicated to health care are mostly provided by large groups (e.g. insurance companies) or by public organizations (e.g. regional governments), the perspective usually reflects society as a whole. Decisions about managing health care resources are based on public interest and require the incorporation of society’s preferences and cost-effectiveness analyses. The concerns of individual patients are generally not included. Because of the limited resources available, the macro level decisions address what treatments, tests, medications can be supported to improve or maintain the health of the population at stake. To do so, some other treatments, interventions or medications need to be reduced or terminated. For example, some expensive biologic medications that can benefit a group of patients with cancer might not be approved due the fact that resources could be alternatively used to vaccinate a large percentage of the population from debilitating infectious diseases. By doing so, cancer patients will have shorter life expectancy; on the other hand, the rest of the population will be protected from a transmittable non-lethal disease. These type of decisions are quite controversial and do not take in consideration individual’s values or preferences as decision makers need to consider that is best for the largest number of individuals.
Meso Level
The level below the macro level is also known as the meso level. It pertains to the clinical decisions involved in the development of guidelines or protocols that can be used for the treatment of specific conditions or for groups of patients with similar diseases. One of the examples on how decisions are made at the mesolevel is provided by the American Society of Colon and Rectal Surgeons who created a standard practice task force that had the main assignment of developing practice parameters for the surveillance and follow-up of patients with colon and rectal cancer [34]. The aim of decision-making at the meso level is to decide on optimal treatment policies. From this point of view, patient preference is important but not essential [27].
Micro Level
The fourth level is called the micro level and applies to decision making at the level of each individual patient. At this stage, patient’s personal preferences are elicited and incorporated. The micro level forms a very important role in the so-called shared decision-making in health-care where clinicians and patients cooperate at selecting treatments that are compatible with individual expectations [35]. Probability Trade Off (PTO) and conjoint analysis (CA) are the two most common instruments developed to study patients’ preferences and measure the strength of their choices [36].
Definition of Utility
The main goal of decision analysis is to make the best decision for each patient. To do so it is important to understand the meaning of patients’ desires and patients’ preferences. Researchers in the field have used the concept of utility that was developed by economists and that can be defined as the level of desirability associated with a particular outcome [37].
Another way of describing utility is an individual patient’s subjective value of a specific health state. Utilities have become a standard measure of value in the analysis of health decisions. There are several methods for attributing utilities to health conditions. Among them, standard gamble, time trade-off, person trade-off, willingness to pay and visual analog scale are the most widely used methods that will be further described in the following paragraphs.
Methods to Measure Desirability for Health States
Standard Gamble (SG)
In the SG method, a subject affected by a disease is asked to choose between two competing outcomes [38,39] The gamble has a probability p of the best possible outcome (optimal health) and a probability (1 – p) of the worst possible outcome (usually immediate death). By varying p, the researcher can measure the value at which the subject is indifferent to the choice between the likely outcome and the gamble. The utility is equal to the value of p at the point of indifference. Let us take as an example a patient affected by end stage renal failure requiring dialysis. If this patient is indifferent to the choice between her/his remaining life on dialysis and a gamble with a probability of 0.90 that her/his remaining life will be in optimal health and a probability of 0.10 of immediate death, the utility of end-stage renal disease is 0.90.
Visual Analog Scale (VAS)
Visual analog scale (VAS) is a rating scale that has the advantage of being easy to use and can be self-administered. Subjects are asked to rate the health state of interest by placing a mark on a 100-mm line where optimal health is represented by the 100 mark and death by the 0 mark. The score is the number of millimeters measured from the death anchor to the mark chosen by the patient, divided by 100. When patients are asked to use the VAS, they do not face any uncertainty or risks. For this reason, VAS and does not reflect any trade-off where an individual is willing to make a sacrifice to achieve better health [40]. An example on how to calculate the utility of the health status of a patients who is affected by claudication is to ask the patient to mark where she/he feels that her/his condition lays between the 0 mark (death) and the 100 mark (walking without any pain). If that patient chooses to mark claudication at the 60 mm mark, that means that the utility associated with that condition is 0.6. However, it is quite possible that if the same patient is asked to gamble between the risk of death that can occur in 40% of cases, and the likelihood of being completely cured that is 60%, she/he might decide that she/he will only accept to gamble if the chance of dying is 10%. That would translate in a utility of 0.9 by using the SG technique.
Time Trade-off (TTO)
In TTO, subjects are asked to choose between their remaining life expectancy in a specific suboptimal health state versus a shorter life lived in perfect health. In other words, they are asked whether they would be willing to trade time of their remaining life to avoid a health problem. In TTO patients’ preferences for a particular health state is quantified by the number of years that patients are willing to trade for an improved health status. For example, participants are asked to consider living in a state of less than full health for a defined period of time (5 or 10 years, depending on their age) and then die. The alternative is to live for a shorter period in full health and then die. The time (x) in full health is varied until the subject is indifferent between the two alternatives. The utility weight for each state is given by the formula x/t [41].
Person Trade-off
Person Trade-off technique is a way of estimating the social value of different health care interventions. Person Trade-off intends to capture the preferences of individuals relative to collective choices that do not directly affect the health status of the individual whose preferences are being elicited. Respondents are asked to imagine that they are decision makers facing a choice between two health care programs. For example, program A would prevent the death of 100 completely healthy individuals thus extending their lives for 10 years. Program B would prevent the onset of a given health problem in some number of healthy people thus improving their health expectancy from 10 years in sub-optimal health to 10 years in ideal health. The subjects are then asked to identify the number of averted health problems considered equivalent to the prevention of 100 deaths [42]. For example, a person is asked to choose between using resources to initiate a campaign that would prevent deaths from car accidents for 100 healthy people who will live another 10 years versus a transplant program that would help patients to be free from hemodialysis for 10 years. This technique is appealing for resource allocation as participants are asked very directly to decide what sacrifices they are prepared to make in the lives of some people in order to provide health benefits to some other people. Although the person trade-off is an intuitively appealing technique for health care decisions where trade-offs are inevitable, it is relatively undeveloped and untested as a valuation technique [43].
Willingness to pay (WTP)
This method has been developed in the context of cost-benefit analysis [44,45]. The direct measurement of WTP uses survey methods to elicit monetary values that can be used to improve personal health. It estimates individuals’ maximum willingness to pay to secure the implementation of a program, diagnostic tests or treatments that could improve the health care status of a person or a group of patients.
Limitations and Strengths of the Instruments Used In Health-Care Decision Making
Standard Gamble, Time Trade-Off, Visual Analog Scale, Willingness to Pay
SG, TTO, VAS and WTP have all been used in decision making studies [46] and all of them have been shown to be feasible and reliable [30] but are cognitively complex and subjects often do not behave according to expected utility theory in real life [47]. It is important to keep in mind that the choice of using any of these methods depends on their aspects of validity. The SG is considered the gold standard in clinical decision making because it is based on uncertainty about the desired outcome [28]. With respect to face validity, the TTO is considered the most valid method because the question it poses is most closely associated with the sort of health care choices that need to be made [42,48]. This holds for many situations in oncology, in which trade-offs between quality of life and length of life are involved and immediate risk is not an issue. In situations in which immediate risk is involved, then the most appropriate method with respect to face validity is the SG. However, a disadvantage of the SG is that the use of probabilities is cognitively complex for the subjects and may lead to biased utilities due to probability distortion [49].
The VAS is appropriate if neither risk nor trade-offs between quality of life and length of life is involved and if weighing different dimensions of quality of life is the only aim. For example, many subjects who indicate a score of less than 100 on a VAS are unwilling to trade life years (in a time trade-off interview) or risk of death (in standard gamble interview) as their condition is perceived as less than optimal but still very good and therefore not worth gambling with the risk of dying while pursuing perfect health [50,51]
Similarly, WTP is association with large variation in subjects’ responses that compromises its discriminant validity. Often individuals are keen to accept large potential costs for healthcare benefits. WTP holds conceptual promise but more empirical research is needed before it can become recognized as a valid and reliable measurement tool. Another limitation of both Person Trade-off and the WTP is that they do not assess health state utilities and have been used primarily for the purpose of making allocation of resources at the societal decision level.
Techniques that Can Be Used In Studies on Clinical Decision Making Assessing Patients’ Preferences for Competing Treatments
Probability Trade-Off
For single patient’s decision making regarding competing treatments, limitations of classic utility assessment tools (e.g. SG, TTO and VAS) have led to the development of alternative methods [52,53]. In clinical medicine most treatment-related health states are only temporary and the elicitation of utilities for these transitory, non-chronic health states is much more complicated than for chronic, stable states [39,54]. SG, TTO and VAS methods are not sufficiently reliable for decision-making for individual patients [55]. This means that individual patient decision-making cannot be based on absolute utility scores and patient’s preferences have to be assessed at individual level by using other techniques [51].
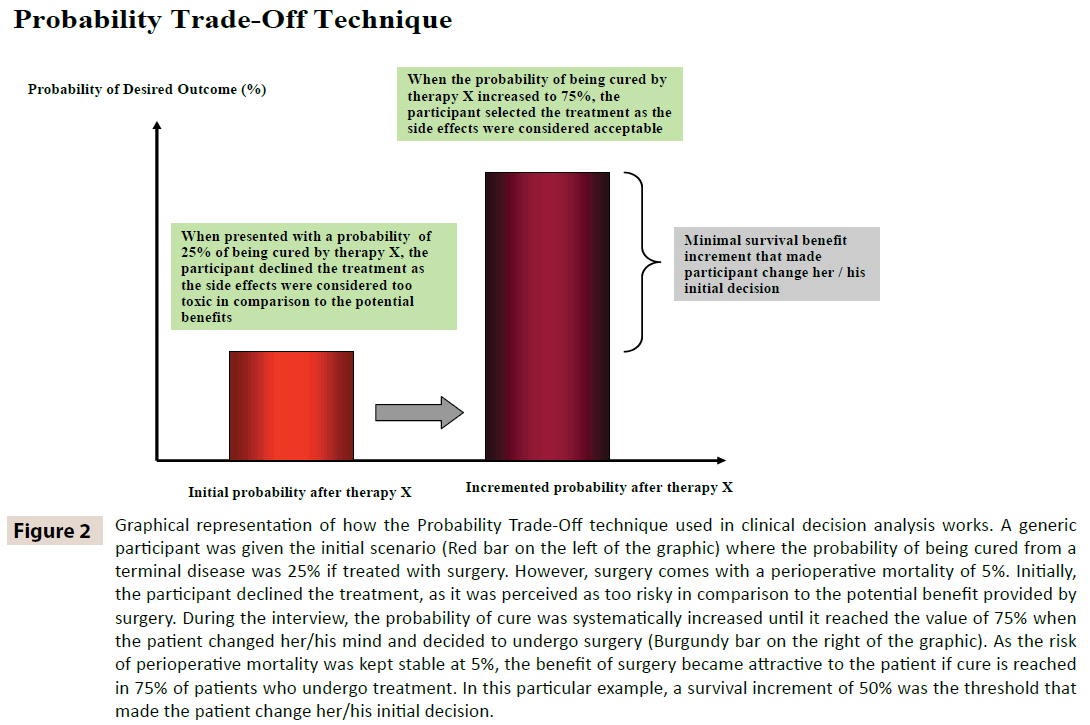
The probability trade off (PTO) method [36] utilizes standardized instructions, visual and verbal information to inform patients about competing treatments and it is able to determine how strongly individuals adhere to their treatment preferences [53]. Patients undergoing PTO interviews receive information about the type and duration of a potential therapy, its side effects and the probability of their occurrence, the likelihood of success or failure at a given time after treatment [56]. This information is presented side-by-side on the same page for ease of comparison. Additional props may be used to explain probabilities better (i.e. a ninety percent chance of survival may be illustrated by a diagram with ten people, with one darkened in to represent the ten percent who die). Each participant is then asked to choose which treatment she/he prefers after considering the overall treatment, its side effects, and its efficacy (Figure 2). In the condition of equal efficacy, the treatment that is usually chosen is the least toxic. During PTO interview, the next step is to change the probabilities of one outcome for the least preferred treatment, in a predetermined, systematic way in order to make it more attractive (i.e. more efficacious, or less toxic). Then the participant is asked again to choose treatments. At some incremental change in probability, the subject will switch her/ his preference (i.e. chose the more toxic regimen, for a greater treatment efficacy). The probability during which this transition occurs (i.e. the “switch point”) is a measure of the strength of preference for the originally chosen treatment regimen, or in decision analysis terms, the point of uncertainty in the decision making process. The investigator can then subtract the “switch point” percentage from the starting percentage in the scenario, and arrive at an absolute difference in probability that is required to change a patients’ preference from one treatment regimen to another. An example of this task is described next. A participant is shown two treatment regimens, regimen A and B, for the adjuvant treatment of breast cancer. At the beginning of the PTO task, regimen A has no side effects and results in a 75% 5-year survival. Regimen B has a 5% risk of deep venous thrombosis (DVT), and results in a 75% 5-year survival. The participants are asked to choose which treatment they prefer, and the majority will naturally choose regimen A. To show the strength of preference for their original decision, which was based on equal efficacy, and a desire to avoid a risk of DVT, the survival is then increased in predetermined increments (i.e. 1% increments), and at each step, patients are asked which treatment they prefer. So the next step in this example is to increase the survival of regimen B to a 76% 5 year survival, and ask the participant which treatment they prefer. At some probability (i.e. when regimen B provides an 82% survival) the participants will switch their preference to regimen B, and accept a 5% risk of DVT for a gain in survival. Assuming a 1% incremental change, the “switch point” percentage is therefore 81.5% (the midpoint between 81 % and 82%). The minimal required increment of survival (MRIS) in this example is therefore 81.5% minus 76%, which is 5.5%. Therefore, in this example participants would prefer regimen B, when it provides a MRIS of 5.5%, occurring at a probability of 81.5% 5-year survival.
Figure 2: Graphical representation of how the Probability Trade-Off technique used in clinical decision analysis works. A generic participant was given the initial scenario (Red bar on the left of the graphic) where the probability of being cured from a terminal disease was 25% if treated with surgery. However, surgery comes with a perioperative mortality of 5%. Initially, the participant declined the treatment, as it was perceived as too risky in comparison to the potential benefit provided by surgery. During the interview, the probability of cure was systematically increased until it reached the value of 75% when the patient changed her/his mind and decided to undergo surgery (Burgundy bar on the right of the graphic). As the risk of perioperative mortality was kept stable at 5%, the benefit of surgery became attractive to the patient if cure is reached in 75% of patients who undergo treatment. In this particular example, a survival increment of 50% was the threshold that made the patient change her/his initial decision.
One of the strengths of PTO is that it helps patients who wish to participate in the decision-making process to clarify and communicate their values [57] and it can be used at the bedside with the help of decision boards and visual aids that can help physicians to be more transparent and explicit [57].
Conjoint Analysis
PTO technique is an approach that leads itself to the determination of patients’ opinions about clinically relevant differences between treatments. For example in cancer care, PTO techniques can be used to identify the point at which potential participants think that the benefits offered by a new treatment would be worthwhile, given a particular probability of toxicity or sideeffects [58]. However, one of the limitations of PTO techniques is that they apply only to the original decision problem and only the strength of preference for one treatment relative to another is obtained. To overcome some of these limitations, recent studies have used another technique that is able to clarify values for different competing treatments by estimating the relative importance of their characteristics, and the total satisfaction that participants may derive from them [44,59,60].
Conjoint Analysis (CA) originated in market research in 1970s, where it has been employed by companies to establish what factors influence the demand for different commodities and thereby what combinations of such attributes will maximize sales of their products [60]. Rather than directly ask survey respondents what they prefer in a product, or what attributes they find most important, conjoint analysis employs the more realistic context of respondents evaluating potential product profiles.
CA measures trade-offs people make in choosing among several possible treatments and it assumes that their preferences are determined by the utility that individuals gain from their selection. Potential treatments are described by their characteristics or attributes. For each attribute, measurement of participants’ inclinations is obtained by utilizing index numbers that measure how valuable or desirable that particular feature is. The extent to which each individual values that characteristic depends on her or his personal utility. The ideas is that attributes which a respondent is reluctant to give up to switch to another treatment are most likely considered to be of higher utility than features which are quickly given up. Preferences for attributes are elicited by using one of these methods: ranking, rating or discrete choices. With ranking, respondents list the scenarios in order of preference. The rating method requires the respondents to assign a score to each of the scenarios. For discrete choice method, respondents are presented with a number of choices and, for each, they are asked to choose their preferred one. CA is an instrument that can be used to value specific characteristics of competing treatments and it is internally consistent and theoretically valid [61].
Conclusions
Making complex decisions are an essential process in every field of health care where “problem solving” skills are a necessity and familiarity with “decision making” is becoming extremely desirable in modern clinicians [62,63]. Problem solving refers to the “search for the single correct solution to a problem”. This requires expertise from medical training. On the other hand, decision-making is the process of choosing between alternative treatments, and requires the contribution of patients and their families who should offer their values and preferences [62,63].
In contrast to policy makers who are dealing with decisions involving large groups, clinicians make decisions at the individual level (Micro Level). To do so, they need to integrate scientific data with qualitative and subjective notions for each patient (i.e. patients’ specific conditions and inclinations).
When more than one treatment is available or the evidence is not strong, even experienced clinicians can be challenged by the process of selecting which intervention would suit their patients best as patients’ preferences are due to reasons that are quite complex and difficult to measure [64]. In these circumstances, the best instruments that can be used by clinicians either in clinics or at the bedside are PTO interviews and CA.
One of the criticisms of this approach is that there might be conflict between patient autonomy and society’s ability to pay for the care that patients would choose if allowed to select among several options. In other words, if providers let patients choose, they will inevitably choose the most expensive options that are not sustainable, especially in countries where there is nationalized health care or within managed care systems. Contrary to these believes, there is good evidence that increasing patient involvement in decisions could actually decrease costs, as studies have shown that patients who are fully informed about risks and benefits tend to choose less intensive interventions than those recommended by their physicians [65].
In our opinion, one of the most challenging parts in shared decision-making is to find out how much involvement each patient wants or needs. Patients are heterogeneous in their willingness to participate in the decision-making process [66-70] as they have different diseases [69,71], level of education, age and gender etc [72].
Therefore, there continues to be considerable debate about when and to what extent patients should be encouraged to voice their preferences. Some argue that patients should be involved only in preference-sensitive decisions [72]. Other argues that since there are benefits and harms to all treatments, virtually every situation should be viewed as appropriate for patient involvement [74]. Another important aspect of shared decision-making is that patients’ preferences depend, in part, by their own estimate of life expectancy and probability of cure that are often incorrect. Patients usually expect more benefits from their treatments than what expected by their doctors [75]. Therefore, health care providers should continue to use their expertise and counsel their patients to reduce their optimistic bias [76,77]. However, it needs to be kept in mind that unless clinicians start actively eliciting patients’ preferences, most of them will continue to play a passive role because they often overlook the concept of uncertainty, the possibility that different therapies are available to them and that each therapy comes with different known risks and benefits.
We hope that by using some of the techniques described in this review, clinicians and their patients will be able to work together and improve their communication and their ability to make good decisions.
References
- Mahler HI1, Kulik JA (1991) Health care involvement preferences and social-emotional recovery of male coronary-artery-bypass patients. See comment in PubMed Commons below Health Psychol 10: 399-408.
- Holen KD1, Klimstra DS, Hummer A, Gonen M, Conlon K, et al. (2002) Clinical characteristics and outcomes from an institutional series of acinar cell carcinoma of the pancreas and related tumors. See comment in PubMed Commons below J Clin Oncol 20: 4673-4678.
- Orth JE, Stiles WB, Scherwitz L, Hennrikus D, Vallbona C (1987) Patient exposition and provider explanation in routine interviews and hypertensive patients' blood pressure control. Health Psychol. 6:29-42.
- Krantz DS (1980) Cognitive processes and recovery from heart attack: a review and theoretical analysis. See comment in PubMed Commons below J Human Stress 6: 27-38.
- Greenfield S1, Kaplan SH, Ware JE Jr, Yano EM, Frank HJ (1988) Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. See comment in PubMed Commons below J Gen Intern Med 3: 448-457.
- Greenfield S, Kaplan S, Ware JE Jr (1985) Expanding patient involvement in care. Effects on patient outcomes. See comment in PubMed Commons below Ann Intern Med 102: 520-528.
- Kuehn BM (2009) States explore shared decision making. See comment in PubMed Commons below JAMA 301: 2539-2541.
- Kravitz RL, Melnikow J (2001) Engaging patients in medical decision making. See comment in PubMed Commons below BMJ 323: 584-585.
- Sowden A1, Forbes C (2001) On the evidence. Patient information. See comment in PubMed Commons below Health Serv J 111: 36-37.
- Sowden AJ1, Forbes C, Entwistle V, Watt I (2001) Informing, communicating and sharing decisions with people who have cancer. See comment in PubMed Commons below Qual Health Care 10: 193-196.
- Wilde N1, Strauss E, Chelune GJ, Loring DW, Martin RC, et al. (2001) WMS-III performance in patients with temporal lobe epilepsy: group differences and individual classification. See comment in PubMed Commons below J Int NeuropsycholSoc 7: 881-891.
- Kassirer JP (1994) Incorporating patients' preferences into medical decisions. See comment in PubMed Commons below N Engl J Med 330: 1895-1896.
- Florin D1, Dixon J (2004) Public involvement in health care. See comment in PubMed Commons below BMJ 328: 159-161.
- Emanuel LL1, Emanuel EJ (1993) Decisions at the end of life. Guided by communities of patients. See comment in PubMed Commons below Hastings Cent Rep 23: 6-14.
- Emanuel LL1, Barry MJ, Stoeckle JD, Ettelson LM, Emanuel EJ (1991) Advance directives for medical care--a case for greater use. See comment in PubMed Commons below N Engl J Med 324: 889-895.
- Broadwell AW1, Boisaubin EV, Dunn JK, Engelhardt HT Jr (1993) Advance directives on hospital admission: a survey of patient attitudes. See comment in PubMed Commons below South Med J 86: 165-168.
- Mansell D1, Poses RM, Kazis L, Duefield CA (2000) Clinical factors that influence patients' desire for participation in decisions about illness. See comment in PubMed Commons below Arch Intern Med 160: 2991-2996.
- Fairley L1, Dundas R, Leyland AH (2011) The influence of both individual and area based socioeconomic status on temporal trends in Caesarean sections in Scotland 1980-2000. See comment in PubMed Commons below BMC Public Health 11: 330.
- Briesacher BA1, Zhao Y, Madden JM, Zhang F, Adams AS, et al. (2011) Medicare part D and changes in prescription drug use and cost burden: national estimates for the Medicare population, 2000 to 2007. See comment in PubMed Commons below Med Care 49: 834-841.
- McNeil BJ, Weichselbaum R, Pauker SG (1981) Speech and survival: tradeoffs between quality and quantity of life in laryngeal cancer. See comment in PubMed Commons below N Engl J Med 305: 982-987.
- McNeil BJ, Weichselbaum R, Pauker SG (1978) Fallacy of the five-year survival in lung cancer. See comment in PubMed Commons below N Engl J Med 299: 1397-1401.
- Singer PA1, Tasch ES, Stocking C, Rubin S, Siegler M, et al. (1991) Sex or survival: trade-offs between quality and quantity of life. See comment in PubMed Commons below J Clin Oncol 9: 328-334.
- Kodish E1, Lantos J, Stocking C, Singer PA, Siegler M, et al. (1991) Bone marrow transplantation for sickle cell disease. A study of parents' decisions. See comment in PubMed Commons below N Engl J Med 325: 1349-1353.
- Ioannidis JPA LJ (2000) Evidence-Based Medicine: A Quantitative Approach to Decision Making. Decision Making In Health Care - Theory, Psychology, and Applications. 1. Cambridge: Cambridge Unversity Press 110-141.
- Elstein AS1 (2004) On the origins and development of evidence-based medicine and medical decision making. See comment in PubMed Commons below Inflamm Res 53 Suppl 2: S184-189.
- Apkon M1 (2003) Decision analysis and clinical uncertainty. See comment in PubMed Commons below CurrOpinPediatr 15: 272-277.
- Montori VM1, Brito JP1, Murad MH1 (2013) The optimal practice of evidence-based medicine: incorporating patient preferences in practice guidelines. See comment in PubMed Commons below JAMA 310: 2503-2504.
- Sarasin FP1 (1999) Decision analysis and the implementation of evidence-based medicine. See comment in PubMed Commons below QJM 92: 669-671.
- Cillo U1, Spolverato G, Vitale A, Ejaz A, Lonardi S, et al. (2015) Liver Resection for Advanced Intrahepatic Cholangiocarcinoma: A Cost-Utility Analysis. See comment in PubMed Commons below World J Surg 39: 2500-2509.
- Torrance GW (1986) Measurement of health state utilities for economic appraisal. See comment in PubMed Commons below J Health Econ 5: 1-30.
- Sutherland HJ1, Till JE (1993) Quality of life assessments and levels of decision making: differentiating objectives. See comment in PubMed Commons below Qual Life Res 2: 297-303.
- Wortley JT, Lemieux-Charles, L. and Meslin, E.M (1994) Research Methods Used in the Study of Managerial Ethics and Decision Making in Health Care: an Annotated Bibliography. Technical Report No 17 Hospital Management Research Unit: University of Toronto.
- Lemieux-Charles L1, Hall M (1997) When resources are scarce: the impact of three organizational practices on clinician-managers. See comment in PubMed Commons below Health Care Manage Rev 22: 58-69.
- Anthony T, Simmang C, Hyman N, Buie D, Kim D, et al. (2004) Practice parameters for the surveillance and follow-up of patients with colon and rectal cancer. See comment in PubMed Commons below Dis Colon Rectum 47: 807-817.
- Imbrogno S. (1998)A Matrix for Decision Analysis in Macro-Practices. Journal of Community Practice 4:49-67.
- Llewellyn-Thomas H, Sutherland HJ, Tibshirani R, Ciampi A, Till JE, et al. (1982) The measurement of patients' values in medicine. See comment in PubMed Commons below Med Decis Making 2: 449-462.
- Bush J (1984) Relative preference versus relative frequencies in health-related quality of life evaluations. New York, NY: Le Jacq.
- Bass EB1, Steinberg EP, Pitt HA, Griffiths RI, Lillemoe KD, et al. (1994) Comparison of the rating scale and the standard gamble in measuring patient preferences for outcomes of gallstone disease. See comment in PubMed Commons below Med Decis Making 14: 307-314.
- Jansen SJ1, Stiggelbout AM, Wakker PP, VlietVlieland TP, Leer JW, et al. (1998) Patients' utilities for cancer treatments: a study of the chained procedure for the standard gamble and time tradeoff. See comment in PubMed Commons below Med Decis Making 18: 391-399.
- Robinson A1, Dolan P, Williams A (1997) Valuing health status using VAS and TTO: what lies behind the numbers? See comment in PubMed Commons below SocSci Med 45: 1289-1297.
- Chou R1, Bürgin H, Schmitt G, Eggers H (1997) Absorption of tretinoin in rats and rabbits following oral and dermal application. See comment in PubMed Commons below Arzneimittelforschung 47: 401-405.
- Salomon JA1, Murray CJ (2004) A multi-method approach to measuring health-state valuations. See comment in PubMed Commons below Health Econ 13: 281-290.
- Green C1 (2001) On the societal value of health care: what do we know about the person trade-off technique? See comment in PubMed Commons below Health Econ 10: 233-243.
- McIntosh E1, Donaldson C, Ryan M (1999) Recent advances in the methods of cost-benefit analysis in healthcare. Matching the art to the science. See comment in PubMed Commons below Pharmacoeconomics 15: 357-367.
- Ryan M1, Ratcliffe J, Tucker J (1997) Using willingness to pay to value alternative models of antenatal care. See comment in PubMed Commons below SocSci Med 44: 371-380.
- Nord E1 (1992) Methods for quality adjustment of life years. See comment in PubMed Commons below SocSci Med 34: 559-569.
- Stiggelbout AM1, de Haes JC (2001) Patient preference for cancer therapy: an overview of measurement approaches. See comment in PubMed Commons below J Clin Oncol 19: 220-230.
- Wang NS1, Ma WL, Zhao HQ, Wei M, Zhang B, et al. (2010) [Survey of the evolutionary characteristics of influenza H1N1 hemagglutinin gene HA1 in 2000-2009]. See comment in PubMed Commons below Nan Fang Yi Ke Da Xue Xue Bao 30: 92-95.
- Wakker P1, Stiggelbout A (1995) Explaining distortions in utility elicitation through the rank-dependent model for risky choices. See comment in PubMed Commons below Med Decis Making 15: 180-186.
- McKee M1 (2010) The World Health Report 2000: 10 years on. See comment in PubMed Commons below Health Policy Plan 25: 346-348.
- Stiggelbout AM1, Eijkemans MJ, Kiebert GM, Kievit J, Leer JW, et al. (1996) The 'utility' of the visual analog scale in medical decision making and technology assessment. Is it an alternative to the time trade-off? See comment in PubMed Commons below Int J Technol Assess Health Care 12: 291-298.
- Llewellyn-Thomas HA1, Williams JI, Levy L, Naylor CD (1996) Using a trade-off technique to assess patients' treatment preferences for benign prostatic hyperplasia. See comment in PubMed Commons below Med Decis Making 16: 262-282.
- Llewellyn-Thomas HA1 (1997) Investigating patients' preferences for different treatment options. See comment in PubMed Commons below Can J Nurs Res 29: 45-64.
- Johnston K1, Brown J, Gerard K, O'Hanlon M, Morton A (1998) Valuing temporary and chronic health states associated with breast screening. See comment in PubMed Commons below SocSci Med 47: 213-222.
- Nunnally JC Bernstein, I H (1994) Psychometric Theory. (3rd Edn) New York, NY: Mcgraw-Hill.
- Llewellyn-Thomas HA, Naylor CD, O'Connor AM (1993) Eliciting patient preferences. See comment in PubMed Commons below Ann Intern Med 118: 76.
- Kiebert GM1, Stiggelbout AM, Kievit J, Leer JW, van de Velde CJ, et al. (1994) Choices in oncology: factors that influence patients' treatment preference. See comment in PubMed Commons below Qual Life Res 3: 175-182.
- Naylor CD1, Llewellyn-Thomas HA (1994) Can there be a more patient-centred approach to determining clinically important effect sizes for randomized treatment trials? See comment in PubMed Commons below J Clin Epidemiol 47: 787-795.
- Pieterse AH1, Stiggelbout AM, Marijnen CA (2010) Methodologic evaluation of adaptive conjoint analysis to assess patient preferences: an application in oncology. See comment in PubMed Commons below Health Expect 13: 392-405.
- Ryan M1, Hughes J (1997) Using conjoint analysis to assess women's preferences for miscarriage management. See comment in PubMed Commons below Health Econ 6: 261-273.
- Propper C (1991) Contingent valuation of time spent on NHS waiting lists. Economic Journal 100:193-199.
- Deber RB1 (1994) Physicians in health care management: 8. The patient-physician partnership: decision making, problem solving and the desire to participate. See comment in PubMed Commons below CMAJ 151: 423-427.
- Deber RB1 (1994) Physicians in health care management: 7. The patient-physician partnership: changing roles and the desire for information. See comment in PubMed Commons below CMAJ 151: 171-176.
- Redelmeier DA1, Rozin P, Kahneman D (1993) Understanding patients' decisions. Cognitive and emotional perspectives. See comment in PubMed Commons below JAMA 270: 72-76.
- Dolan P1 (1999) Whose preferences count? See comment in PubMed Commons below Med Decis Making 19: 482-486.
- Bruera E1, Sweeney C, Calder K, Palmer L, Benisch-Tolley S (2001) Patient preferences versus physician perceptions of treatment decisions in cancer care. See comment in PubMed Commons below J Clin Oncol 19: 2883-2885.
- Cassileth BR, Zupkis RV, Sutton-Smith K, March V (1980) Information and participation preferences among cancer patients. See comment in PubMed Commons below Ann Intern Med 92: 832-836.
- Cassileth BR, Zupkis RV, Sutton-Smith K, March V (1980) Informed consent -- why are its goals imperfectly realized? See comment in PubMed Commons below N Engl J Med 302: 896-900.
- Degner LF1, Kristjanson LJ, Bowman D, Sloan JA, Carriere KC, et al. (1997) Information needs and decisional preferences in women with breast cancer. See comment in PubMed Commons below JAMA 277: 1485-1492.
- Elkin EB1, Kim SH, Casper ES, Kissane DW, Schrag D (2007) Desire for information and involvement in treatment decisions: elderly cancer patients' preferences and their physicians' perceptions. See comment in PubMed Commons below J Clin Oncol 25: 5275-5280.
- Rothenbacher D1, Lutz MP, Porzsolt F (1997) Treatment decisions in palliative cancer care: patients' preferences for involvement and doctors' knowledge about it. See comment in PubMed Commons below Eur J Cancer 33: 1184-1189.
- Pieterse AH1, Baas-Thijssen MC, Marijnen CA, Stiggelbout AM (2008) Clinician and cancer patient views on patient participation in treatment decision-making: a quantitative and qualitative exploration. See comment in PubMed Commons below Br J Cancer 99: 875-882.
- Zandbelt LC1, Smets EM, Oort FJ, Godfried MH, de Haes HC (2007) Patient participation in the medical specialist encounter: does physicians' patient-centred communication matter? See comment in PubMed Commons below Patient EducCouns 65: 396-406.
- McNutt RA1 (2004) Shared medical decision making: problems, process, progress. See comment in PubMed Commons below JAMA 292: 2516-2518.
- Weeks JC1, Cook EF, O'Day SJ, Peterson LM, Wenger N, et al. (1998) Relationship between cancer patients' predictions of prognosis and their treatment preferences. See comment in PubMed Commons below JAMA 279: 1709-1714.
- Fraenkel L1, McGraw S (2007) Participation in medical decision making: the patients' perspective. See comment in PubMed Commons below Med Decis Making 27: 533-538.
- Paradis C1 (2008) Bias in surgical research. See comment in PubMed Commons below Ann Surg 248: 180-188.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences