Collateral Pathways in Budd Chiari Syndrome- MDCT Depiction
Chauhan U,Goel V, Jain N,Raj N, Singh M and Puri SK
DOI10.4172/2472-1891.100025
Chauhan U*, Goel V, Jain N, Raj N, Singh M and Puri SK
Department of Radiology, Govind Ballabh Pant Institute of Post Graduate Medical Education and Research, New Delhi, India
- *Corresponding Author:
- Chauhan U
Department of Radiology, Govind Ballabh
Pant Institute of Post Graduate Medical
Education and Research, New Delhi, India.
Tel: 01123234242
E-mail: dr.udit.chauhan@gmail.com
Received: March 25, 2016; Accepted: May 12, 2016; Published: May 20, 2016
Citation: Chauhan U, Goel V, Jain N, et al. Collateral Pathways in Budd Chiari Syndrome-MDCT Depiction. Int J Dig Dis.2016, 2:2. doi:10.4172/2472-1891.1000025
Abstract
Budd Chiari syndrome (BCS) is a condition arising from hepatic venous outflow tract obstruction (HVOTO) arising at the level of hepatic veins, inferior vena cava, right atrium or a combination of these. It can be classified as primary or secondary depending upon the underlying pathophysiology. Regardless of the cause of HVOTO, there is lack/complete absence of hepatic venous drainage leading to constellation of symptoms pertaining to portal hypertension with radiologically visible intrahepatic and extrahepatic porto-systemic collaterals. The presence of these collateral systems provide imaging diagnostic clue in chronic cases with cirrhosis labelled as chronic liver disease and thereby establishing the primary cause of cirrhosis to be BCS. Current essay aims to provide in depth knowledge of collateral pathways of BCS.
Keywords
Budd Chiari syndrome; Thrombosis; Hypertension; Chronic; Liver
Introduction
Budd Chiari syndrome (BCS) is a condition arising from hepatic venous outflow tract obstruction (HVOTO) arising at the level of hepatic veins, inferior vena cava, right atrium or a combination of these. It can be classified as primary or secondary depending upon the underlying pathophysiology. Epidemiologically the causes of primary BCS in western countries include the hepatic venous thrombosis/IVC thrombosis due to systemic disease in contrast to membranous or segmental obstruction of IVC in the Asian countries. Secondary causes by far remain similar like malignant obstructing masses or compressing mass lesions, etc. [1,2] Regardless of the cause of HVOTO, there is lack/complete absence of hepatic venous drainage leading to constellation of symptoms pertaining to portal hypertension with radiologically visible intrahepatic and extra hepatic porto-systemic collaterals [3]. The presence of these collateral systems provide imaging diagnostic clue in chronic cases with cirrhosis labelled as chronic liver disease and thereby establishing the primary cause of cirrhosis to be BCS. Therefore the knowledge of these collateral pathways is essential in order to achieve correct diagnosis of BCS so as to allow for timely intervention. The primary aim of this essay is to describe the collateral pathways seen on MDCT (Multi Detector Computed Tomography) venography of abdomen. We present the current essay from the case of a 25 year old female patient diagnosed as chronic liver disease (CLD) presenting with pain abdomen, ascites and deranged liver functions with a history of single episode of upper GI bleed. Viral markers were negative and diagnosis of cryptogenic CLD was sought for till the CECT abdomen revealed it to be case of chronic Budd Chiari syndrome with extensive venous collateralisation.
Materials and Method
A CT examination was conducted on a 256 slice, dual source CTmodel SOMATOM Definition FLASH. CECT (contrast enhanced computed tomography) abdomen was performed from the dome of diaphragm till the pelvic outlet. NCCT (noncontrast computed tomography) scan was done prior to triple phase scan of the abdomen which consisted of arterial, porto venous and delayed phases. The phases were obtained with empirically timed scans using a bolus injector with arterial phase obtained between 20- 30 s, portovenous/hepatic venous phase 60-70 s and delayed phase at 120 s. The injection rate was between 3.5-4 ml/s and contrast injection was followed by saline chase 30 ml at the rate of 3 ml/s. 80 ml of contrast was given for the study.
Collateral pathways in Budd Chiari syndrome: multiple collateral path ways have been described in BCS. These could be intrahepatic or extra hepatic.
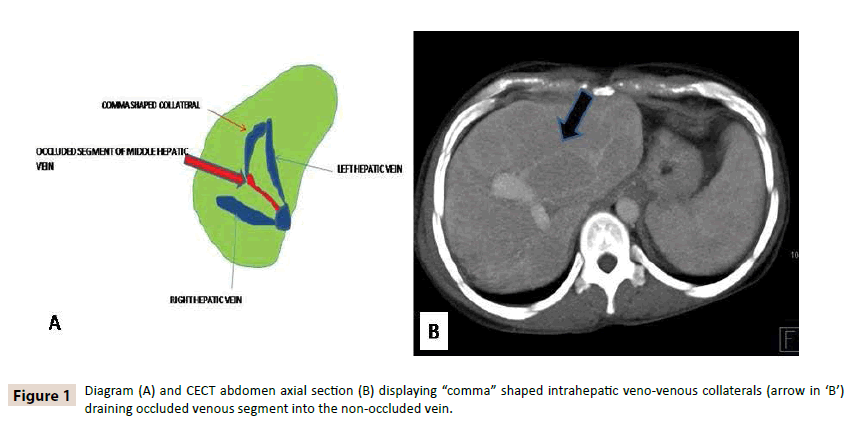
1) Intrahepatic collaterals: Two forms of intrahepatic collaterals are seen
• Those that drain into the systemic veins through subcapsular venous plexus and
• Those that shunt the segment of occluded vein into the nonoccluded venous segment and are seen as “comma” shaped veno-venous collaterals. These are best seen on sonography [4] (Figure 1).
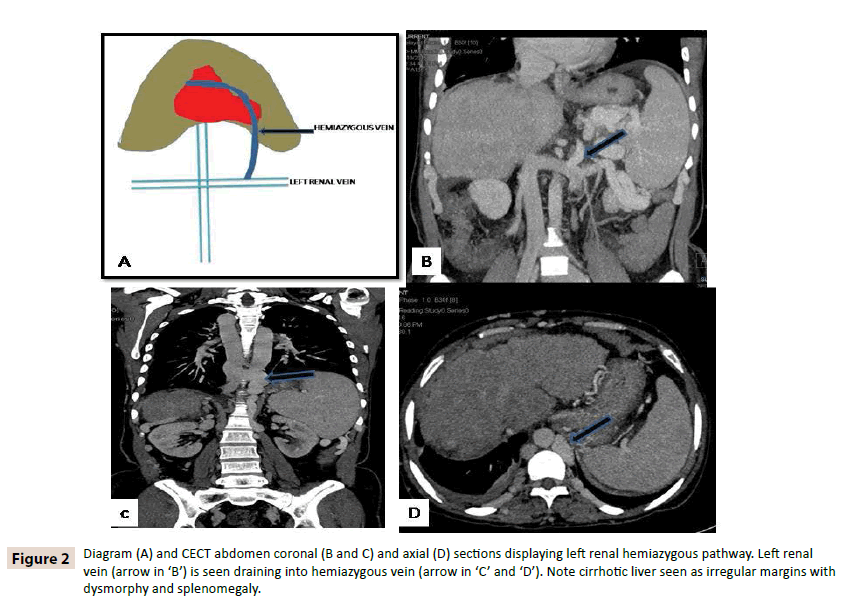
2) Left renal hemiazygous pathway
Left renal vein has complex anatomy due to the fact that many veins like inferior phrenic, gonadal and adrenal veins drain into it. Left renal vein communicates with the retroperitoneal veins namely lumbar, ascending lumbar and hemiazygous vein. These communications ultimately reach into the right atrium. This drainage pathway can form the major drainage pathway in the cases of BCS [5] (Figure 2).
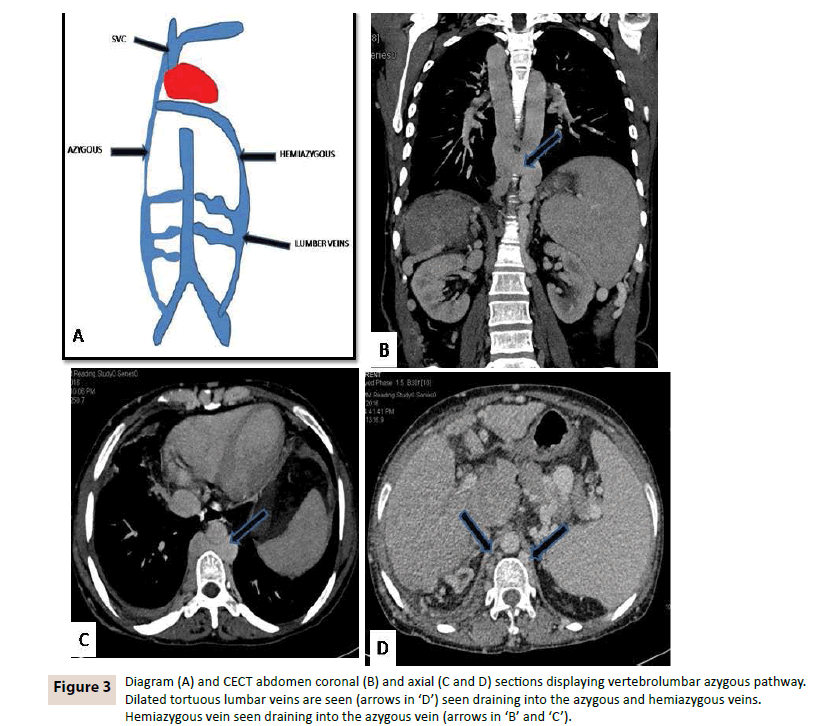
3) Vertebrolumbar azygous pathway
Flow in the IVC could reverse and reach common iliac vein and then into the ascending lumbar veins thereby draining into the azygous vein. Ascending lumbar veins are seen parallel to the spine and poster lateral to the aorta and IVC. Reversal of flow could be seen in the gonadal or ureteric veins towards the common iliac vein and then into the azygous system [2]. It is the most common collateral pathway in BCS (Figure 3).
Figure 3: Diagram (A) and CECT abdomen coronal (B) and axial (C and D) sections displaying vertebrolumbar azygous pathway. Dilated tortuous lumbar veins are seen (arrows in ‘D’) seen draining into the azygous and hemiazygous veins. Hemiazygous vein seen draining into the azygous vein (arrows in ‘B’ and ‘C’).
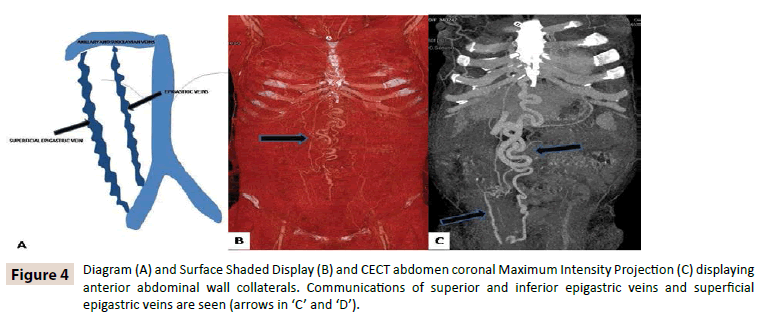
4) Anterior abdominal wall collaterals
• The collaterals comprising this system include one between the superior and inferior epigastric veins and other between the superficial epigastric and lateral thoracic veins.
• Inferior epigastric vein arises from the external iliac vein joins superior epigastric vein above the level of umbilicus to drain into the subclavian vein and ultimately right heart.
• Flow may also follow the common femoral vein through superficial circumflex iliac vein to superficial epigastric vein and anastomosing with the lateral thoracic vein.
• Collaterals comprising the superior and inferior epigastric communications are seen medially in contrast to the posterolaterally situated superficial epigastric and lateral thoracic veins. The laterally situated superficial epigastric veins are seen clinically as caput medusa [6] (Figure 4).
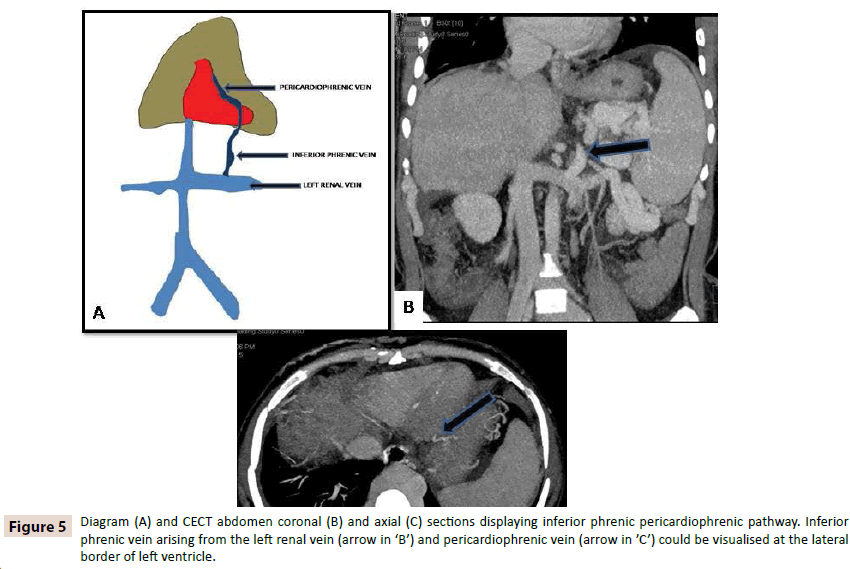
5) Inferior phrenic pericardio-phrenic collaterals
• Pericardiophrenic vein is a tributary of the left brachiocephalic vein and has communications with inferior phrenic vein. Inferior phrenic vein on right side drains into the IVC while on left side can drain into the IVC and into the left renal vein. Left hepatic vein and left phrenic vein have ostia close to each other. Sometimes left phrenic vein can drain into the left hepatic vein. This pathway drains the intrahepatic collaterals into the phrenic vein and then into the pericardiophrenic vein (Figure 5).
Figure 5: Diagram (A) and CECT abdomen coronal (B) and axial (C) sections displaying inferior phrenic pericardiophrenic pathway. Inferior phrenic vein arising from the left renal vein (arrow in ‘B’) and pericardiophrenic vein (arrow in ’C’) could be visualised at the lateral border of left ventricle.
• Thus it is clear from above essay that the collateral pathways in the BCS are quite characteristic and are easy to recognise if carefully sought for. These have importance as they help to ascertain the cause of cirrhosis to BCS and allow for appropriate treatment which may include interventional radiological procedure (like hepatic venous stenting or direct intrahepatic portosystemic shunt - DIPS) or surgery.
Treatment options in budd chiari syndrome
1. Caval recanalization: Caval recanalisation is the best option if feasible in the patients with caval obstruction. A large diameter balloon is used to dilate the segment [7].
2. Hepatic vein recanalization: In cases with hepatic venous obstruction recanalisation of the native or accessory hepatic veins is done in order to establish the hepatic venous outflow. Balloon dilatation with or without angioplasty and stent placement remains the treatment option [7].
3. Portosystemic shunt creation (TIPS/DIPS): In cases when the hepatic veins are replaced by multiple intrahepatic collaterals restoration of hepatic outflow in not possible by recanalisation/cavoplasty. In such cases portosystemic shunt is created through transjuglar route either as transjuglar intrahepatic portosystemic shunt (TIPS) or direct portocaval shunt. In cases if the notch is seen from the IVC to suggest possible hepatic venous and IVC junction a TIPS is done else DIPS is performed [7,8].
4. Surgery: Surgical shunt creation is no longer considered an option for BCS due better midterm results of interventional procedures. In cases with end stage liver disease or fulminant hepatic failure the definitive treatment is liver transplant [7].
References
- Lim JH, Park JH, Auh YH (1992)Membranous obstruction of the inferior vena cava: comparison of findings at sonography, CT and venography.AJR Am J Roentgenol 159:515-520.
- Sonin AH, MajerMi (1992) Powers TA. Obstruction of the inferior vena cava: a multiple modality demonstration of causes, manifestations and collateral pathways. RadioGraphics 12:309-322.
- Janssen HL, Garcia-Pagan JC, Elias E (2003) Budd-Chiari syndrome: a review by an expert panel. J Hepatol 38:364-371.
- Redmond PL,Kadir S, Cameron JL (1988) Transhepatic collaterals in a patient with the Budd-Chiari syndrome. Cardiovasc Iriterrent Rwliol 11: 285-287.
- Abrams HL (1983) Angiography vascular and interventional radiology. (3rdedn) I.Boston: Little, Brownpp: 950-958.
- Pagaini I, Thomas JL,Berhardino ME (1982) Computed tomographic manifestations of abdominal and pelvic venous collaterals. Radiology 142:415-419.
- Al-Warraky MA, TharwaBE, Kohla BM, Aljaky BMA, Aziz CA (2015) Evaluation of different radiological interventional treatments of Budd–Chiari syndrome.The Egyptian Journal of Radiology and Nuclear Medicine 46: 1011-1020.
- Anders N, Stine A, Dennis N, Peter H, Vilstrup H et al. (2013) Treatment of Budd– Chiari syndrome with a focus on transjugular intrahepatic portosystemicshunt. World J Hepatol 5: 38-42.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences