Helicobacter pylori seropositivity in England, 2001-2007: time trends and the effect of ethnicity
Kalliopi Alexandropoulou,Fiona Reid,Richard Holliman, Hasan Al-Ghusein,Andrew Poullis,Jin-Yong Kang
DOI10.4172/2472-1891.100006
Kalliopi Alexandropoulou1, Fiona Reid2, Richard Holliman3, Hasan Al-Ghusein3, Andrew Poullis4 and Jin-Yong Kang4*
1Department of Gastroenterology, Guildford Hospital
2Department of Medial Statistics, St George’s Hospital, London
3Department of Clinical Microbiology, St George’s Hospital, London
4Department of Gastroenterology, St George’s Hospital, London
- *Corresponding Author:
- Jin-Yong Kang
Department of Gastroenterology, Knightsbridge Wing
St George’s Hospital, Blackshaw Rd, London SW17 0QT
Fax: 0044 208 725 3520
E-mail: jykang@sgul.ac.uk
Citation: Jin-Yong Kang, et al. Helicobacter pylori seropositivity in England, 2001-2007: time trends and the effect of ethnicity. Int J Dig Dis. 2015, 1:1. doi:10.4172/2472-1891.100006
Abstract
Background: Helicobacter pylori (HP) prevalence is decreasing in developed countries. Widespread adoption of the 'test and treat' strategy for dyspepsia (2002) may have contributed to this decline.
Methods: Time trends in the proportion of positive HP serology results in our institution, covering an ethnically diverse area in London, were analysed between 2001 and 2007. The effect of age, gender and ethnicity was assessed.
Results: 12307 tests were carried out between 2001 and 2007 in 11484 consecutive patients. There was a statistically significant reduction in the proportion of positive tests over the study period from 42.8% to 37.6% (p<0.001). HP seroprevalence was higher in older individuals (p<0.001), in men (p=0.001) and in patients of Indian subcontinent descent (p<0.001). There was a fall in the proportion of positive tests to HP over time for both genders and ethnic groups and among patients over age 30. The proportion of positive tests to HP remained unchanged for younger individuals.
Conclusion: The proportion of positive HP serology in our institution decreased over a seven-year period. HP infection was more prevalent in older patients. A significant proportion of younger subjects had positive HP serology but the seroprevalence of HP infection amongst subjects aged under 30 remained unchanged.
Keywords
Helicobacter pylori epidemiology; Seroprevalence; Race/ ethnicity
Introduction
Helicobacter pylori (HP) infection occurs in asymptomatic individuals but is also a major cause of common gastrointestinal diseases [1] including peptic ulcer and gastric cancer, conditions which have declined in incidence world-wide [2]. This decline parallels a fall in the prevalence of HP infection in both developed [3,4] and developing countries [5,6]. By contrast, there is a negative association between HP infection and gastro-oesophageal reflux disease [7] a condition which, although less common in the Orient than in the west [8], is increasing in frequency worldwide [9]. Oesophageal adenocarcinoma, a complication of chronic gastro-oesophageal reflux is also increasing in prevalence [10,11]. Since Helicobacter pylori infection has a negative association with oesophageal adenocarcinoma [12], a decline in the prevalence of HP infection may have undesirable effects.
HP infection is usually acquired at an early age [13] and associated with poor socio-economic conditions during childhood [5,14]. In developing countries, early childhood infection results in a peak of HP prevalence rates in early adulthood [15], while in developed countries the age-associated prevalence rate plateaus off only among the elderly [16]. It has previously been thought that the increasing seroprevalence of HP infection with age in developed countries is the result of a birth cohort phenomenon, due to infection being acquired primarily in childhood and persisting throughout life, unless eradication treatment is given. Older subjects who experienced poorer socio-economic conditions in their childhood were more likely to be infected with HP compared to individuals from subsequent generations. The prevalence of HP infection and peptic ulcer is therefore higher in older birth cohorts compared to those born in later decades, when socioeconomic conditions have improved [3,4].
The incidence of HP infection includes both primary infection and re-infection after successful eradication, with a low annual incidence of 0.5-1.0% for adults in developed countries, compared to higher rates of 3-10% in developing countries [17]. Prospective longitudinal studies of HP prevalence show that the flux between HP sero-conversion and sero-reversion may be more significant than was previously thought [5,18-20].
Within developed countries, HP infection rates tend to be higher amongst immigrant populations [5,19,20] reflecting high childhood acquisition rates in their countries of origin as well as poorer living conditions even in their adopted countries [19].
The gold standard for diagnosing HP infection remains biopsy based tests [21]. Non-invasive urea breath testing and stool antigen testing are used clinically but are relatively costly. Most epidemiological studies rely on serology, which, although low in specificity, provides the most practical method of studying large populations and allows the use of previously stored sera. However HP serology reflects previous exposure to infection rather than active infection. Although HP seropositivity tends to revert after successful HP eradication the rate of reversion is variable and up to 65% of patients remained sero-positive more than a year after successful eradication [22]. Serology is therefore an inadequate tool in assessing the dynamic relationship between HP seroconversion and sero-reversion. However, it remains a valid tool in assessing the prevalence of HP infection in a community.
Our institution serves a large ethnically diverse population across South West London, England, where 80% of people describe themselves as White, 8% Asian, 7% Black and 5% of mixed or other ethnic origin [23]. This population has varying levels of social deprivation [23].
The aim of the present study was to determine, over a 7-year period from 2001 to 2007, the proportion of positive results for HP serology, with particular reference to age, gender and Indian subcontinent ethnicity. This is a period of particular interest, with recent introduction of effective chemotherapy regimens for HP eradication and the ‘test and treat’ strategy for HP in the management of dyspepsia, in place since 2002.
Methods
Our laboratory used an automated qualitative enzyme linked fluorescent assay for measuring HP IgG levels, recording results as positive, negative or equivocal. Data from 2001 to 2007 were analysed to determine the frequency of positive serology for HP. For patients who were tested more than once during the study period, our analysis considered only the first result. Data on patient age, gender and ethnicity were recorded. As ethnic group is not routinely recorded in our hospital records, patients’ names were used as a surrogate marker to identify individuals of Indian subcontinent Asian descent, using a previously validated approach [24]. The remaining subjects were considered as ‘other ethnic groups’.
Statistical Analysis
Logistic regression was used (SPSS package, version 16) to examine the change in HP seropositivity over time, adjusted for effects of age, gender and ethnicity. Further logistic regression analysis was carried out to investigate effect of age, gender and ethnicity on HP seropositivity, with calculated odds ratios adjusted in each case for all other variables. A p-value of <0.05 was considered as statistically significant.
Results
HP serology was performed on 12307 specimens from 11484 patients. Six hundred and fifty eight patients were tested twice, 62 patients three times, 9 patients four times, 2 patients five times and one patient was tested 6 times during the study period. Gender was not recorded in 161 cases (78 HP +ve, 48%) and date of birth in 41 (21 HP +ve, 51%). There were 4949 men (44%) and 6374 women (56%). 8898 patients (77.5%) were aged 50 years or less. Two thousand, one hundred and six subjects (18.3%) were of Indian subcontinent Asian ethnicity. The proportion of patients with Indian subcontinent ethnicity was similar across the seven years of the study, while the proportion of females increased slightly, and the mean age varied but showed no clear time trend.
The proportion of positive HP tests fell over the seven year study period, from 42.8% in 2001 to 37.6% in 2007 (Table 1). Higher HP infection rates were significantly associated with increasing age, male gender, and Indian subcontinent Asian ethnicity (Table 2). Indian subcontinent Asian patients, who accounted for 18.3% of the study cohort, were twice as likely to be positive for HP serology compared to other ethnic groups combined (95% CI 2.01- 2.44, p <0.001).
| Year | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 |
|---|---|---|---|---|---|---|---|
| Total patients tested | 1503 | 1664 | 1389 | 1448 | 1721 | 1969 | 1790 |
| Mean Age | 41 | 42 | 37 | 35 | 39 | 42 | 42 |
| Age Range | 3-100 | 2-92 | 4-87 | 3-89 | 4-90 | 3-93 | 2-97 |
| Total HP seropositive | 643 | 724 | 539 | 559 | 664 | 769 | 673 |
| % HP seropositive | 42.8 | 43.5 | 38.8 | 38.6 | 38.6 | 39.1 | 37.6 |
| Men | 684 | 724 | 638 | 614 | 762 | 795 | 732 |
| % Seropositive men | 45.2 | 44.3 | 37.3 | 43.3 | 40.7 | 40.9 | 40.2 |
| Indian subcontinent Asians | 277 | 299 | 274 | 284 | 276 | 392 | 304 |
| % Seropositive Indian Subcontinent Asians |
59.6 | 55.5 | 62.0 | 56.0 | 54.3 | 51.5 | 49.3 |
Table 1: Number of patients tested over the study period.
| Variable | OddsRatio | 95%*CI | P value |
|---|---|---|---|
| Year Tested | 0.962 | 0.944, 0.981 | <0.001 |
| Age (per year) | 1.022 | 1.020, 1.025 | <0.001 |
| Male gender | 1.142 | 1.057, 1.235 | <0.002 |
| Indian subcontinent Asians | 2.213 | 2.006, 2.442 | <0.001 |
Table 2: Odds Ratios for HP seropositivity for included study variables (logistic regression model)
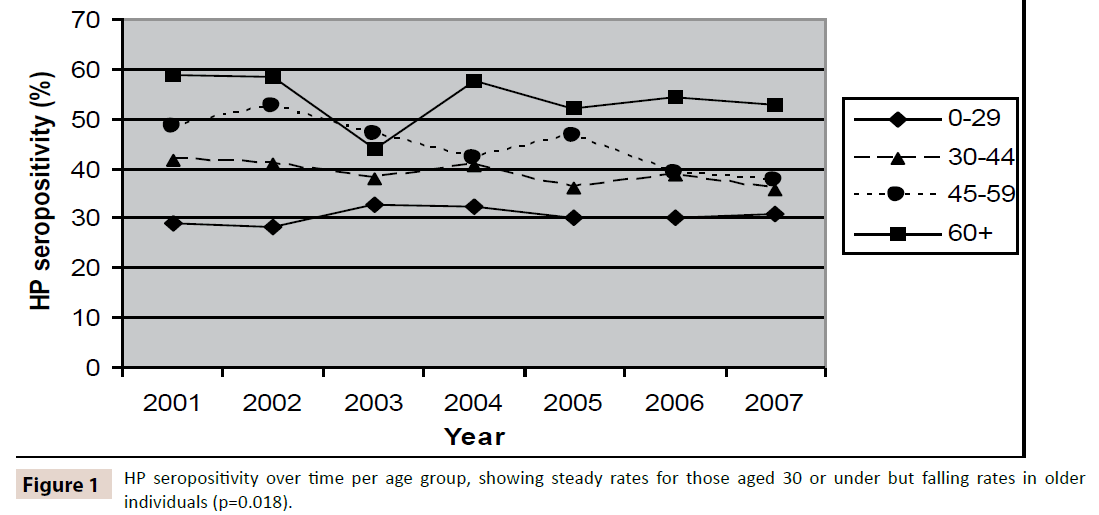
A further logistic regression model tested for interactions between the variables. The proportion of positive tests for HP fell over time among older individuals but remained stable in those aged under 30 years (n=2926), with 29.2% positive for HP in 2001 compared with 31.1% in 2007 (Figure 1, p=0.018).
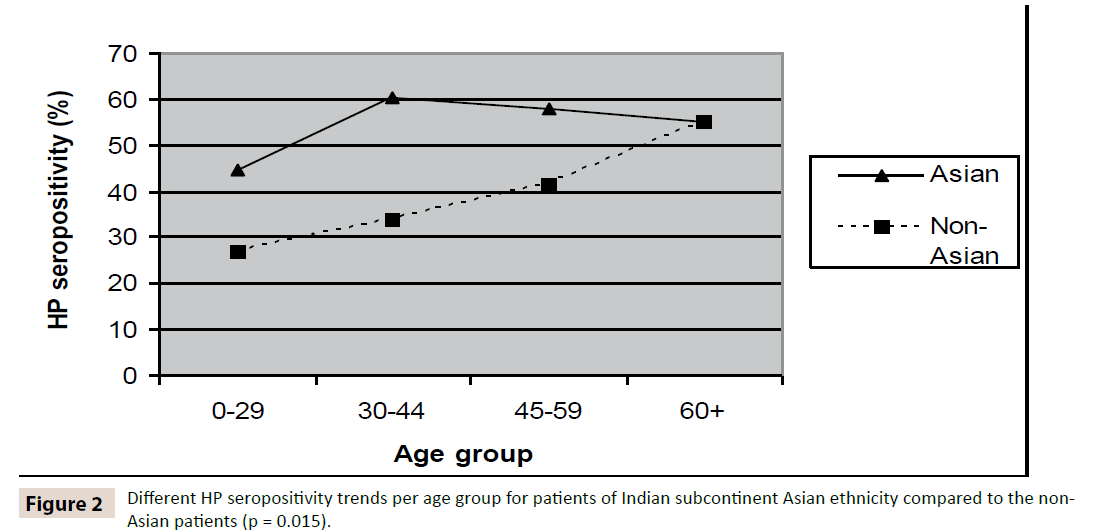
There was also an interaction between age and ethnicity. HP infection rates increased steadily with age among non-Asian subjects as expected, but while rates among Asians aged 30- 44 were higher than for those aged under 30 years, they were similar to those aged above 55 (Figure 2, p=0.015). Over the study period HP seroprevalence fell more sharply amongst those from an Indian-subcontinent Asian background compared to the others, but this difference just failed to reach statistical significance (p= 0.051).
Seven hundred and thirty-three patients were tested on more than one occasion. On initial testing of these 733 patients, there were 274 (37%) positive results, 387 (53%) negative results while 72 patients (9.8%) had equivocal results. On repeat testing, persistent HP seropositivity was seen in 209 (76.3%) of the 274 originally HP sero-positive patients. In 41 patients (15%) the serology results had reverted to negative while in 24 patients (8.7%) an equivocal result was obtained on the second occasion. Of the 387 patients who were sero-negative on initial testing, 348 (90%) remained sero-negative on second testing but new positive results were obtained in 30 (7.8%) patients.
Discussion
The prevalence of HP infection in the general population in England and Wales, estimated using HP serology was 14% in 1996, but higher in London than in other regions [25] .Our results show higher levels of HP seropositivity as compared to the general population, which is perhaps to be expected since most of our patients were likely to have presented with dyspepsia and since our patients include a high proportion of men, older individuals and Indian sub-continent Asians, all these being risk factors for HP infection, compared to the total population of the United Kingdom [5,19,20,26].
The frequency of positive HP serology in our samples declined over a 7-year period. The population in London is more ethnically diverse than the overall British population but the trend we described occurred in both Indian sub-continent Asians and non- Asians alike. A 7 year period seems too short for the decrease to be explained by the classical model of a birth cohort effect influenced by improved socio-economic conditions in successive generations. There was no change for those aged under 30 years, consistent with stable childhood socio-economic conditions for these individuals and the likelihood that new immigrants are likely to be older individuals. The fall in HP seropositivity among patients aged 30 years and above suggests a role for other agerelated factors, such as exposure to antibiotics and/or proton pump inhibitors. Rapid recent declines in HP seroprevalence rates have been reported from several other countries. A study from South China showed a significant decrease in HP seroprevalence between 1993 and 2003, ranging from 11.4% to 18% in different age groups [27]. Two cross-sectional studies from St Petersburg, Russia also identified a marked reduction in HP seroprevalence in children, from 44% to 13%, between 1995 and 2005 [28]. These changes were attributed to improvement in the standard of living but widespread use of HP eradication therapy, as well as spontaneous elimination of infection, were also cited as contributing factors.
In a Greek study, adult patients attending a gastroenterology clinic in 1987 had a lower seroprevalence of 49.2%, compared to 59.5% for a cohort of patients who attended in 1987 [29]. Higher HP prevalence was seen in those born in the 1940s, during a period of war-time deprivation.
Malaty et al followed up 644 Japanese children and adults from 1986 to 1994 [30] and carried out two independent crosssectional surveys in the same population over the same time period [30,31]. Although seropositivity increased with age within each cross-sectional study, the overall prevalence declined over the study period from 32% to 17% in children and from 87% to 74% in adults. The incidence (sero-conversion) and loss (seroreversion) rates for HP infection were 1.1% and 1.8% respectively in children and 1% and 1.5% in adults. Specific HP eradication therapy was not used during the study period and the authors attributed the falling sero-prevalence to antibiotic exposure for incidental infections. A Dutch study on gastric biopsy specimens from 11691 consecutive patients undergoing endoscopy from 1992 to 2001, found higher HP prevalence rates in immigrants (77% M: 72% F) compared to the indigenous population (35%M: 32% F), and in men compared to women. The prevalence for both groups declined over the study period [20].
HP infection is associated with lower socio-economic status in adulthood even after adjustment for childhood socio-economic conditions [32]. Socio-economic factors are likely to have also contributed to the overall higher HP seroprevalence in Indiansubcontinent Asians. Improved socio-economic circumstances following immigration may have led to the plateau in HP seropositivity found in our older Asian subjects, since these individuals are likely to have lived in the United Kingdom and be exposed to British living standards longer than younger Asians subjects in our study.
Racial differences in HP prevalence have been reported. Higher HP prevalence amongst Black Americans as compared to White Americans [14,33] among Singapore Chinese and Indians compared to Malays [34,35] and also the Dutch study cited above. Multiple factors probably contribute to these differences, including socio-economic conditions, cultural practices and possibly genetic factors [36]. In the present study, HP positivity rates for Asians aged 30 and above, some of whom may well have spent their childhood abroad, were comparable to non-Asians aged 60 and above. By contrast, younger Asians, some of who are probably second generation immigrants born in the UK, had HP positivity rates intermediate between younger non-Asians and Asians aged 30 and above.
There are several weaknesses to our study. The specimens do not come from a representative community sample, but from symptomatic patients. However, population studies have shown similar HP infection rates in patients with and without dyspepsia [37,38] so our analysis may indeed reflect HP rates in our catchment population to some extent.
We used commercial serological test kits which were not specifically validated in our population. Serological testing after specific HP eradication treatment would be expected to lead to fewer positive results as HP serology may revert from positive to negative, although antibody titres fall slowly and may still be present 4 years after successful eradication [21]. For this reason, serological testing for HP infection is only recommended for the initial evaluation of dyspepsia, and not for monitoring the effectiveness of eradication treatment. However, some doctors may not have been knowledgeable about these guidelines and a proportion of patients may have had repeat HP serology requested inappropriately to evaluate the effect of treatment. Other patients may have sought medical advice for dyspeptic symptoms on more than one occasion, potentially confounding our results. To reduce the impact of these confounding factors, we analysed only the initial HP serology result for each patient.
HP testing for dyspeptic patients without ‘alarm’ symptoms such as unintentional weight loss and dysphagia was introduced in the 1990s to reduce the need for endoscopy, but these guidelines were subsequently amended. The earliest guidelines suggested a ‘test and treat’ strategy for patients aged under 45 years. It was recommended that older dyspeptic patients be investigated by endoscopy because of the higher frequency of pathology in older individuals. In 2002, the age limit below which the ‘test and treat’ policy applied was raised to 55 years while the latest National Institute of Clinical Excellence (NICE) guidelines recommended HP testing as the initial step in the algorithm for the investigation of dyspepsia in patients of any age as long as ‘alarm’ symptoms are absent [39]. It was therefore expected that the demography of patients undergoing HP serology testing would become older over the study period with the proportion of positive HP serology results also increasing for this reason. However our study population did not show an increase in age over time.
Conclusions
The most likely explanation for our results is a significant rate of serological reversion, through more frequent HP eradication. Although specific anti-HP therapy would have been a factor, it cannot be the whole explanation since most patients would have been tested prior to treatment rather than after. Instead, our results are more likely to be due to use of antibiotics for other indications, and would be consistent with the more rapid fall in HP seropositivity observed in the older age groups of the Indian Subcontinent Asian patients. Proton pump inhibitors have an anti-HP effect [40] and are synergistic when combined with antibiotics for HP eradication, as in standard triple therapy. The use of proton pump inhibitors have increased greatly in recent years [41] and this could have contributed to the results seen in the present study.
In conclusion, the frequency of positive results for HP serology in a London laboratory declined significantly over a 7-year period. While the reasons for this decrease are not entirely clear, one possibility is that reversion of HP serology is occurring in a significant number of subjects. The classical view that the decline in HP infection in western countries is due to a birth-cohort phenomenon alone may have to be revised.
References
- Blaser MJ (1998) Helicobacter pylori and gastric diseases. BMJ 316:1507-1510.
- El Serag HB, Sonnenberg A (1998) Opposing time trends of peptic ulcer and reflux disease. Gut 43:327-333.
- Roosendaal R, Kuipers EJ, Buitenwerf J, van Uffelen C, Meuwissen SG et al. (1997) Helicobacter pylori and the birth cohort effect: evidence of a continuous decrease of infection rates in childhood. American Journal of Gastroenterology 92:1480-1482.
- Banatvala N, Mayo K, Megraud F, R. Jennings,J J Deeks et al. (1993) The cohort effect and Helicobacter pylori. Journal of Infectious Diseases 168:219-221.
- Malaty HM (2007) Epidemiology of Helicobacter pylori infection. Best Practice & Research in Clinical Gastroenterology 21:205-214.
- Xia HH, Talley NJ, (1997) Natural acquisition and spontaneous elimination of Helicobacter pylori infection: clinical implications. American Journal of Gastroenterology 92:1780-1787.
- Weston AP, Badr AS, Topalovski M, Rachel C, Anita D et al. (2000) Prospective evaluation of the prevalence of gastric Helicobacter pylori infection in patients with GERD, Barrett's esophagus, Barrett's dysplasia, and Barrett's adenocarcinoma. American Journal of Gastroenterology 95:387-394.
- Dent J, el Serag HB, Wallander MA, Johansson S. (2005) Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 54:710-717.
- El Serag HB (2007) Time trends of gastroesophageal reflux disease: a systematic review. Clinical Gastroenterology & Hepatology 5:17-26.
- Devesa SS, Blot WJ, Fraumeni JF Jr (1998) Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer 83:2049-2053.
- Newnham A, Quinn MJ, Babb P, Kang JY, Majeed A (2003) Trends in oesophageal and gastric cancer incidence, mortality and survival in England and Wales 1971-1998/1999. Alimentary Pharmacology & Therapeutics 17:655-664.
- De MC, Llosa AE, Farr SM,Gary D. Friedman, Joseph H V et al. (2005) Helicobacter pylori infection and the risk of development of esophageal adenocarcinoma. Journal of Infectious Diseases 191:761-767.
- Malaty HM, El Kasabany A, Graham DY, Miller CC, Reddy SG et al. (2002) Age at acquisition of Helicobacter pylori infection: a follow-up study from infancy to adulthood. Lancet 359:931-935.
- Graham DY, Malaty HM, Evans DG, Evans DJ Jr, Klein PD et al. (1991) Epidemiology of Helicobacter pylori in an asymptomatic population in the United States. Effect of age, race, and socioeconomic status. Gastroenterology 100:1495-1501.
- Graham DY, Adam E, Reddy GT, Jai P A, Rohit A et al. (1991) Seroepidemiology of Helicobacter pylori infection in India. Comparison of developing and developed countries. Digestive Diseases & Sciences 36:1084-1088.
- Pounder RE, Ng D (1995) Theprevalence of Helicobacter pylori infection in different countries. Alimentary Pharmacology& Therapeutics 9:33-39.
- Parsonnet J (1995) The incidence of Helicobacter pylori infection. Alimentary Pharmacology& Therapeutics 9:45-51.
- Rosenstock S.J., Andersen L.P., Bonnevie O., et al. (1996) Sero-conversion and sero-reversion in IgG antibodies to H pylori: An 11 year follow up of 2,523 randomly selected Danes. GUT 39
- De Vries AC, Van Driel HF, Richardus JH,Martine Ouwendijk, Adriana J. Van Vuuren et al. (2008) Migrant communities constitute a possible target population for primary prevention of Helicobacter pylori-related complications in low incidence countries. Scandinavian Journal of Gastroenterology 43:403-409.
- Loffeld RJ, van der Putten AB (2003) Changes in prevalence of Helicobacter pylori infection in two groups of patients undergoing endoscopy and living in the same region in the Netherlands. Scandinavian Journal of Gastroenterology 38:938-941.
- Dzierzanowska F K, Lehours P, Megraud F, Dzierzanowska D (2006) Diagnosis of Helicobacter pylori infection. Helicobacter 11:6-13.
- Cutler AF, Prasad VM (1996) Long-term follow-up of Helicobacter pylori serology after successful eradication. American Journal of Gastroenterology 91:85-88.
- Health and the 2001 Census: South West London. NHS Publication.
- Strachan DP, Powell KJ, Thaker A, Millard FJ, Maxwell JD (1995) Vegetarian diet as a risk factor for tuberculosis in immigrant south London Asians. Thorax 50:175-180.
- Vyse AJ, Gay NJ, Hesketh LM, Andrews NJ, Marshall B et al. (2002) The burden of Helicobacter pylori infection in England and Wales. Epidemiology & Infection 128:411-417.
- De Martel C, Parsonnet J (2006) Helicobacter pylori infection and gender: a meta-analysis of population-based prevalence surveys. Digestive Diseases & Sciences 51:2292-2301.
- Chen J, Bu XL, Wang QY, Hu PJ, Chen MH (2007) Decreasing seroprevalence of Helicobacter pylori infection during 1993-2003 in Guangzhou, southern China. Helicobacter 12:164-169.
- Tkachenko MA, Zhannat NZ, Erman LV, Blashenkova EL, Isachenko SV et al. (2007) Dramatic changes in the prevalence of Helicobacter pylori infection during childhood: a 10-year follow-up study in Russia. Journal of Pediatric Gastroenterology & Nutrition 45:428-432.
- Apostolopoulos P, Vafiadis-Zouboulis I, Tzivras M,Kourtessas D, Katsilambros N et al. (2002) Helicobacter pylori (H pylori) infection in Greece: the changing prevalence during a ten-year period and its antigenic profile. BMC Gastroenterology 2:11.
- Kumagai T, Malaty HM, Graham DY, Hosogaya S, Misawa K et al. (1998) Acquisition versus loss of Helicobacter pylori infection in Japan: results from an 8-year birth cohort study. Journal of Infectious Diseases 178:717-721.
- Malaty HM, Kumagai T, Tanaka E, Ota H, Kiyosawa K et al. (2000) Evidence from a nine-year birth cohort study in Japan of transmission pathways of Helicobacter pylori infection. Journal of Clinical Microbiology 38:1971-1973.
- Moayyedi P, Axon AT, Feltbower R, Duffett S, Crocombe W et al. (2002) Relation of adult lifestyle and socioeconomic factors to the prevalence of Helicobacter pylori infection. International Journal of Epidemiology 31:624-631.
- Malaty HM, Graham DY, Wattigney WA, Srinivasan SR, Osato M et al. (1999) Natural history of Helicobacter pylori infection in childhood: 12-year follow-up cohort study in a biracial community. Clinical Infectious Diseases 28:279-282.
- Ho KY, Chan YH, Kang JY (2005) Increasing trend of reflux esophagitis and decreasing trend of Helicobacter pylori infection in patients from a multiethnic Asian country. American Journal of Gastroenterology 100:1923-1928.
- Kang JY, Yeoh KG, Ho KY, Guan R, Lim TP et al. (1997) Racial differences in Helicobacter pylori seroprevalence in Singapore: correlation with differences in peptic ulcer frequency. Journal of Gastroenterology & Hepatology 12: 655-659.
- Malaty HM, Engstrand L, Pedersen NL, Graham DY (1994) Helicobacter pylori Infection: Genetic and Environmental nfluences: A Study of Twins. Annals of Internal Medicine120: 982-986.
- Parsonnet J, Blaser MJ, Perez-Perez GI, Hargrett-Bean N, Tauxe RV (1992) Symptoms and risk factors of Helicobacter pylori infection in a cohort of epidemiologists. Gastroenterology 102:41-46.
- Talley NJ, Hunt RH (1997)What role does Helicobacter pylori play in dyspepsia and nonnuclear dyspepsia? Arguments for and against H. pylori being associated with dyspeptic symptoms. Gastroenterology 113: S67-77.
- NICE. National Institute for Clinical Excellence. Dyspepsia: Managing dyspepsia in adults in primary care. Centre for Health Services Research Report No 112. University of Newcastle upon Tyne, 2004.
- Peterson WL (1997)The role of antisecretory drugs in the treatment of Helicobacter pylori infection. Alimentary Pharmacology & Therapeutics 1:21-25.
- Martin RM, Lim AG, Kerry SM, Hilton SR (1998) Trends in prescribing H2-receptor antagonists and proton pump inhibitors in primary care. Alimentary Pharmacology & Therapeutics 12:797-805.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences