Critical Analysis of ALPPS Procedure: A Single Centre Experience
Peteja M, Vávra P, Pelikán A, Lerch M, Ihnát P, ZonÄÂÂa P, Janout V and Elgendi A
DOI10.4172/2472-1891.100032
Peteja M1,2*, Vávra P1,2, Pelikán A1,2,4,5, Lerch M1,2, Ihnát P1,2, ZonÃÆââ¬Å¾ÃâÃÂa P1,6, Janout V3 and Elgendi A7
1Department of Surgery, University Hospital Ostrava, Czech Republic
2Department of Surgical Studies, University of Ostrava, Czech Republic
3Department of Epidemiology and Public Health, University of Ostrava, Czech Republic 4St. Mary‘s Hospital Newport, Isle of Wight, UK
4St. Mary‘s Hospital Newport, Isle of Wight, UK
5Department of Health Care Sciences, Tomas Bata University in Zlín, Czech Republic
6Surgical Center, Ostrava, Czech Republic
7Department of Surgery, Alexandria University, Egypt
- *Corresponding Author:
- Peteja M
Department of Surgery
University Hospital Ostrava, Czech Republic
Tel: +420 602 774 546
E-mail: anton.pelikan@fno.cz
Received Date: February 26 , 2018; Accepted Date: March 28, 2018; Published Date: April 09, 2018
Citation: Peteja M, Vávra P, Pelikán A, Lerch M, Ihnát P, et al. (2018) Critical Analysis of ALPPS Procedure: A Single Centre Experience. G J Dig Dis 4:1. doi: 10.4172/2472-1891.100034
Abstract
The ALPPS (Associating Liver Partition and Portal vein Ligation for Staged Hepatectomy) method was presented to the expert public with the intention of providing a chance to patients with metastatic or primary liver cancer and a lack of residual parenchyma excluding resection therapy which is considered to be the only curative treatment. This method has been regarded as controversial due to its high mortality and morbidity on the one hand and high resection success rate on the second hand. The article presents the initial experience from one workplace. Materials and Methods: From August 2013 to June 2014 eight patients were selected for ALPPS method of hepatic resection at the Surgery of the University Hospital Ostrava Czech republic. For all patients the initial FLR (future liver remnant) volume was less than 25% and they have exhausted other treatment options for the disease. Results: The group consisted of two men and six women, aged 40 to 70. Four patients had CRC (colorectal cancer) liver metastases and two patients were diagnosed with gallbladder cancer metastatic to the liver. The first female patient suffered from hilar cholangiocarcinoma and the last female patient had leiomyosarcoma. Altogether six patients were subject to both phases of the therapy (75% of cases). From the entire patient group one female patient died after the first phase due to haemorrhagic shock, and one was assessed by the multidisciplinary team as unsustainable for the second phase. Remaining all six patients who underwent both phases of surgery had R0 resection but three of them had severe liver failure and they ended fatally. Conclusion: ALPPS is a new method for inducing rapid hypertrophy of the liver parenchyma based on the ligation the portal vein branch and in-situ splitting. However this therapy is still burdened by a relatively high rate of morbidity and mortality which are directly related to the tumour’s histological character to the age of the patient and to the functional state of their hepatic parenchyma
Keywords
ALPPS; Liver hypertrophy; In situ splitting; Hepatectomy
Abbreviations
ALPPS: Associating Liver Partition And Portal Vein Ligation For Staged Hepatectomy; CRC: Colorectal Cancer; CRLM: Colorectal Liver Metastasis; CCC: Cholangiocelular Cancer; FLR: Future Liver Remnant; TLV: Total Liver Volume; CT: Computed Tomography; KGR: Kinetic Growth Rate; POD: Postoperative Day; SBRT: Stereotactic Body Radiation Therapy; MODS: Multiorgan Distress Syndrome; HIDA Scan: Cholescintigraphy and Hepatobiliary Scintigraphy; PVE: Portal Vein Embolization; IVC: Inferior Vena Cava
Introduction
Hepatic resection remains the only hope for cure in patients with extensive hepatic metastases or with a large primary liver tumour. Different techniques have been described to induce hypertrophy of hepatic tissues for those patients. ALPPS (Associating Liver Partition and Portal vein Ligation for Staged Hepatectomy) [1,2] is an innovative modification to the traditional two stage hepatectomy combining a hepatic parenchymal transection with portal vein ligation. This the first stage of procedure results in accelerated liver hypertrophy and enabling completion hepatectomy (stage 2) within a short period usually only one to two weeks. Despite these great advantages, ALPPS has been seriously challenged by criticisms due to reported high morbidity and mortality. Even experienced centres have reported high mortality rates up to 20% [3-7].
In this study we are presenting our experience with ALPPS procedure and analyse the outcomes, including survival benefits and procedure related complications.
Material and Methods
From August 2013 to June 2014, eight patients were selected for the ALPPS procedure of hepatic resection at the Surgery of the University Hospital Ostrava. They were two males and six females with age ranging from 40 to 70 years. Four patients (50%) had previously colorectal cancer (CRC) now with liver metastases, two patients had gallbladder cancer with hepatic involvement, one patient had hilar cholangiocarcinoma, and one patient had leiomyosarcoma of the liver.
The selection criteria for ALPPS procedure was based on the preoperative planning by a triphasic CT with the volumetric assessment of the remnant liver volume (FLR-future liver remnant-less than 25%). All patients underwent standardised pre-operative preparation and evaluation of the liver parameters and overall performance status too. Cholescintigraphy and hepatobiliary scintigraphy (HIDA scan) with a normal functional finding was performed in three patients.
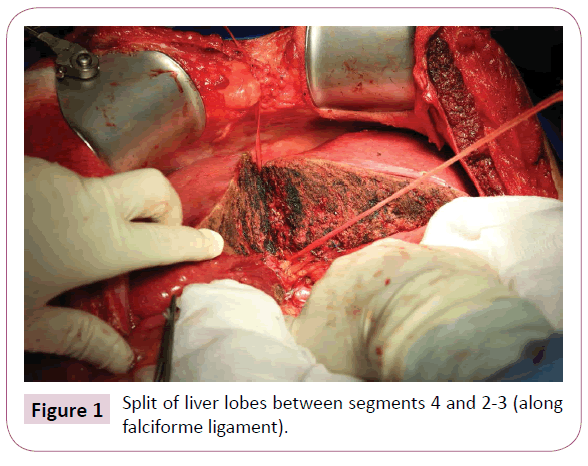
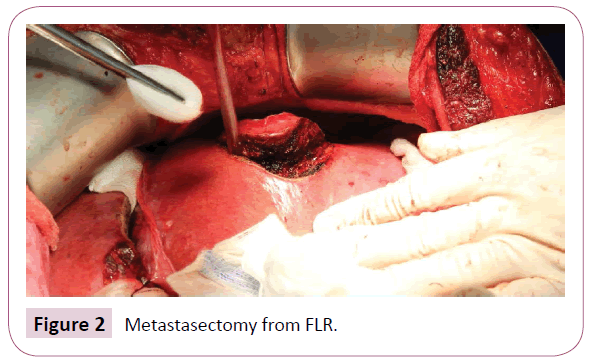
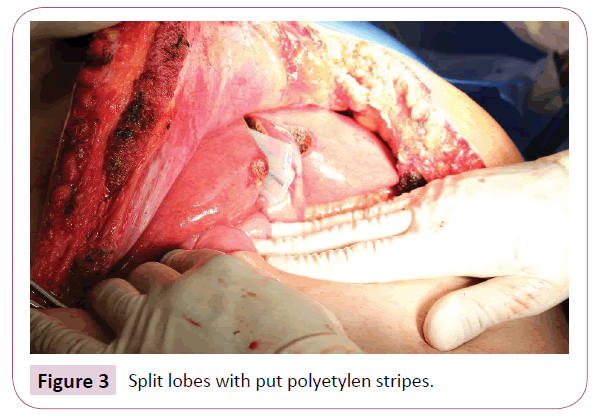
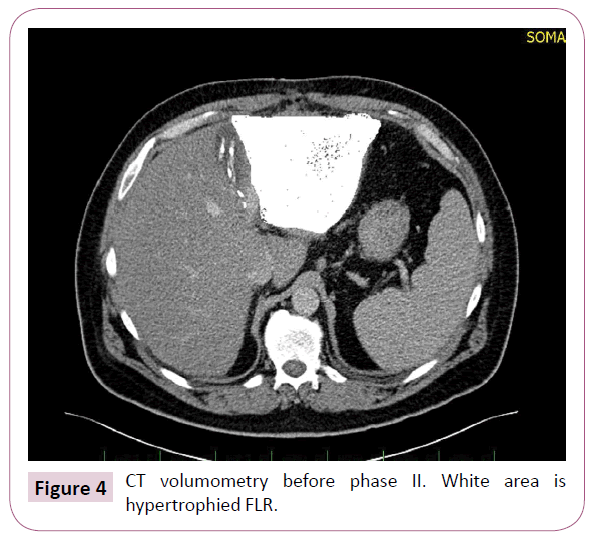
The resection was performed on all patients according to the same operating algorithm. All operation procedures were performed using open approach. A chevron (rooftop) or Mercedes incision was made, liver was completely mobilized, and intraoperative ultrasonography was performed. Then a hepatoduodenal ligament was dissected with using of the Pringle manoeuvre. The right liver was mobilized from the inferior vena cava and the hepatic artery too, the portal vein and the common hepatic duct were prepared. The right portal vein in its distant part to the bifurcation was dissected and sutured, followed by hepatic parenchymal transection. The splitting to the right of the falciform ligament was performed by using the Cavitron Ultrasonic Surgical Aspirator (CUSA) device in combination with a harmonic scalpel (Figure 1). During operation if some metastases were detected in the left liver lobe, they were removed during this the first phase (Figure 2). Resection area was covered with a tape drain (Figure 3). After this operative procedure was conducted the CT scan with volumometry in the range of 10th- 27th day and on its result the next phase was scheduled (Figure 4). The second phase was carried out after ligation and division of the previously prepared structures including the right hepatic artery also the right and middle hepatic veins with the right hepatic duct and the affected lobe was removed. In the post-operative phase, patients were hospitalised at the Intensive and Resuscitation Care Clinic and then depending on their clinical conditions at the appropriate hospital department. Between the two phases, patients were given antibiotics with combinations of parenteral and enteral nutrition. Every patient was followed-up regularly after the operation.
Results
The group consisted of eight patients. Apart from a female patient suffered from liver leiomyosarcoma all remaining patients underwent several cycles of chemotherapy before liver surgery. No pre-operative tests revealed a hepatic failure, haemocagulation pathology or other co-morbidity, which would contraindicate the extensive liver resection.
Pre-operative evaluation of volume parameters showed FLR/ TLV (TLV-total liver volume) ratio in the range 14.6-23%, median value at 18.7% (Table 1). A control CT scan with volumometry was performed for all patients between the 10th till 27th day (median value 13.7) after the first stage operation. The relative increase in FLR volume was 16-105% (median 64.2%). The FLRto- TLV ratio was 30.9% (range 25-40%). The KGR (kinetic growth rate per day) was 12.48 cm³/day and 4.8%/day (7.22-18 cm³/day, 1.3-7.2%/day respectively).
| Cumulative data | |
|---|---|
| Age | 56,1 (43-70) |
| ASA score | 2,6 (II-III) |
| Gender (male/female) | 2/5 |
| BMI | 25,8 (22,8-35,5) |
| Weight (kg) | 73,3 (60-115) |
| Preoperative chemotherapy | 6 (85,7%) |
| Tumor type: | |
| Colorectal liver metastases | 3 (42,9%) |
| Hilar cholangiocarcinoma | 1 (14,3%) |
| Gallbladder cancer | 2 (28,5%) |
| Leiomyosarcoma-liver metastases | 1 (14,3%) |
| Preoperative volume: | |
| TLV (cm3) | 1656 (960-2978) |
| FLR (cm3) | 315 (190-698) |
| FLR/TLV (%) | 18,7 (14,6-23) |
| Volume increase between stage one and two: | |
| FLR (cm3) | 473,7 (385-807) |
| Relative gain in volume (%) | 64,2 (16-105) |
| FLR/TLV | 30,9 (25-40) |
| KGR (cm3/day) | 12,48 (7,22-18) |
| KGR (%/day) | 4,8 (1,3-7,2) |
| Time between Stage I and control CT-volumometry (days) | 13,7 (10-27) |
Table 1: Patients’ data: Personal, tumour type, volume, time line.
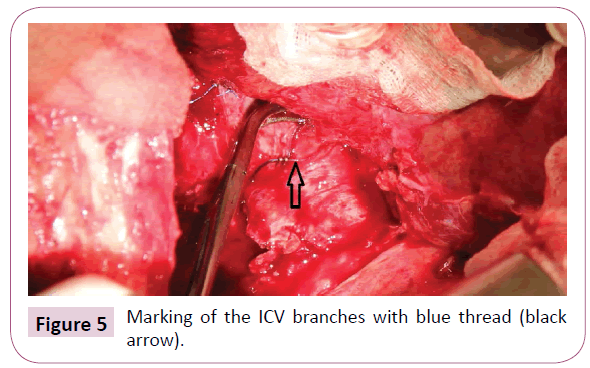
The average operating time of the first phase was 370 minutes (350-420 min) and 230 minutes (110-450 min) for the second phase. Blood loss during the first phase was average 1957 ml (600-5000 ml), and 1683 ml (400-3500 ml) during the second phase (Table 2). Resection of another organ was not carried out on any patient. Colour tapes were used during the first phase to identify structures of the hepatoduodenal ligament and the inferior vena cava (IVC) branches for all patients and tape drains separated resection area of the split lobes (Figure 5).
| Cumulative | Stage I | Stage II | |
|---|---|---|---|
| Operative time (min) | 605 (480-773) | 370 (350-420) | 230 (110-450) |
| Blood loss (ml) | 3400 (2300-5000) | 1957 (600-5000) | 1683 (400-3500) |
| Intraoperative transfusion | 7(100%) | 4 (57%) | 4 (57%) |
Table 2: Operation time and blood loss.
Only six of eight patients completed the two-stage procedure. The reason was for a female patient with a hilar cholangiocarcinoma experienced a severe perioperative bleeding during the first phase and even though the bleeding had been stopped, the patient died of haemorrhagic shock combined with hepatic failure. The second patient with metastatic hepatic disease due to colorectal cancer following her initial phase of the treatment was decided to postpone the next treatment phase for a few weeks because of his psychic failure to manage the proposal for further treatment with the threat of suicide. In remaining six patients, planned operative procedure was performed.
Complications of the procedure were evaluated according to the Dindo-Clavien classification [8]. In the post-operative phase, three patients developed a severe liver failure followed by the hepatorenal syndrome with multiorgan distress syndrome (MODS) and finally with their death. Deterioration of the condition occurred on the 12th, 4th and 9th postoperative day and subsequent death on 14th, 11th and 13th post-operative day. Adding the female patient who died of haemorrhagic shock, four patients suffered Grade V complication according to Dindo- Clavien. Two of the deceased patients had gallbladder carcinoma, one cholangiocellular carcinoma, and one female patient suffered from metastatic disease based on colorectal cancer.
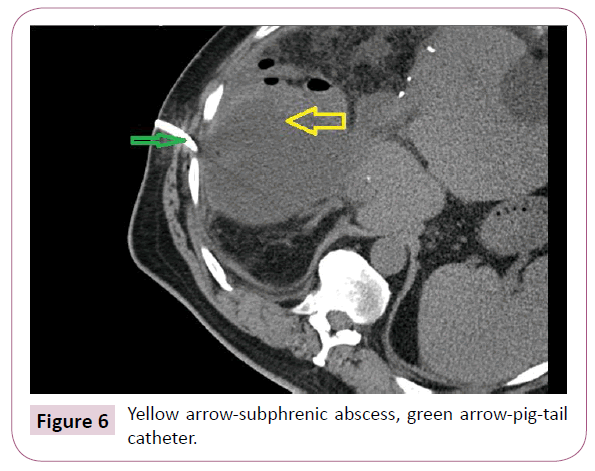
As far as the remaining three patients and their complications are concerned: A subphrenic biliary collection was diagnosed in one patient what required drainage under CT guidance (Figure 6) – a IIIA-complication, and skin sutures had to be dissolved in one female patient due to the presence of a subcutaneous abscess- Grade I complication. R0 resection was achieved in all patients.
Oncological Outcomes
Out of three patients who successfully completed both stages of ALPPS procedure, the female patient with leiomyosarcoma enjoyed a disease-free interval of 18 months, then the disease re-occurred, and the patient died 29 months after the second phase. The patient with colorectal carcinoma metastasis is currently alive 48 months after ALPPS. However, 15 months after the removal of liver metastases, a recurrence in the descendentrecto anastomosis was detected. Resection and reanastomosis was performed. The patient lived without any complaints for another 15 months when a recurrence of metastases in residual hepatic parenchymal was detected. Currently, the patient is receiving a SBRT (CyberKnife) treatment. More recently, peritoneal carcinomatosis was diagnosed but he is still alive. In the last female patient with the metastatic liver disease due to CRC, metastases in lungs and subsequently in the remaining liver was detected 6 months after the ALPPS. Palliative chemotherapy was offered to her but she died 16 months after the second phase.
Discussion
The resection R0-is the main treatment option available at achieving cure in patients with metastatic colorectal liver cancer or a large primary hepatic tumour. Not infrequently, the volume of the future liver remnant after resection is not enough. Inducing hypertrophy of the liver is a well-known phenomenon that has been practiced since two decades. This can be achieved by embolization or ligation of the right or left portal blood flow [9]. However, these procedures also run the risk of tumour progression between the time of embolization and resection [3,10].
The time taken between inducing hypertrophy and resection during ALPPS procedure can be reduced to 10-14 days when compared with 6 weeks in portal vein embolization. This may reduce the risk of further metastatic disease [11,12]. The rate of liver hypertrophy for ALPPS (the combination of ligation of the right portal branch, hepatic parenchymal transection and devascularisation of segment IV) is superior to the portal vein occlusion or embolization [4]. In concordance with the data available in the published literature we were able to induce rapid hypertrophy to the left lateral section and were able to perform resection in our patients, however three patients died from hepatic failure.
The procedure ALPPS is associated with many advantages in liver surgery but early mortality remains a serious problem for this newly practiced surgical technique. Even experienced hepatobiliary centres have reported high 90-day mortality rates ranging between 10% and 20% [1,3-5].
In various malignancies, hepatic metastases are very often the cause of death following R0 resection of a primary tumour and statistics report that 80% of CRC patients are diagnosed with synchronous or metachronous metastases [7]. The only curative procedure for these patients is surgical treatment; however, this treatment requires a minimal residual volume of the hepatic parenchyma to prevent the occurrence of liver failure which has fatal consequences. Established FLR hypertrophy-inducing procedures fail in 30% of patients due to too lengthy process of hypertrophy, during which the disease progresses [3,7,12,13]. The ALPPS method aims to target this disadvantage because the interval between the first and second phases is shortened here to 7-10 days. Unfortunately, such rapid induction of the hypertrophic mechanisms is paid with higher mortality and morbidity rates [3,4,13].
Our group of patients has demonstrated various types of malignancies, both CRLM (colorectal cancer liver metastasis) and CCC (cholangiocelular cancer), gallbladder cancer or leiomyosarcoma metastases. Also, the age structure of the patients was different. In all patients, the R0 resection was achieved. One female patient was excluded from the statistics because a multidisciplinary evaluation following the first stage had assessed her as unsustainable to the next stage; she was released home where she committed suicide. Another female patient with presumed metastasis of a gynaecological tumour had suffered from a massive perioperative bleeding, and even though it was stopped, a severe haemorrhagic shock subsequently developed with fatal consequences. Histologically, it was a cholangiocellular cancer. Three patients completed both phases in good condition, but they all suffered from a severe liver failure (on 14th, 4th or 9th post-operative day) that ended with death. Three patients successfully completed both stages of ALLPs procedure. Two patients had uneventful recovery; however one patient developed a biliary collection in right sub-phrenic space that was percutaneously drained under CT scan guidance.
Conclusion
Although APPLS procedure provides an alternate to overcome drawbacks of traditional two stage hepatectomies involving portal vein embolization, the morbidity and mortality rates remain high. The initial popularity of ALPPS procedure appears to be fading away due to associated complications. The total number of patients in our series is small and a larger prospective study is required to evaluate disease free survival benefit over acceptable morbidity and mortality.
We believe this procedure should continue to be a part of surgeon’s armamentarium, however a more thorough risk assessment, patient’s performance status, disease burden and selection criteria are key to successful outcome.
The fact that the patient with colorectal liver metastases enjoyed a 30-month disease-free interval, as far as hepatic failure is concerned, gives us the hope that this malignancy in the younger patient represents the accurate ALPPS indication. However, our written statement does not have the weight and the basis of the study, it points to the modest experience of one workplace where the implementation of the surgical method is going through some difficulties.
References
- Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, et al. (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 255: 405–414.
- de Santibanes E, Clavien PA (2012) Playing Play-Doh to prevent post-operative liver failure: the ‘‘ALPPS’’ approach. Ann Surg 255: 415–417.
- Li J, Girotti P, Konigsrainer I, , Ladurner R, Königsrainer A, et al. (2013) ALPPS in right trisectionectomy: a safe procedure to avoid postoperative liver failure? J Gastrointest Surg 17: 956-961.
- Schadde E, Ardiles V, Slankamenac K, Tschuor C, Sergeant G, et al. (2014) ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg 38: 1510–1519.
- Nadalin S, CapobiancoI, Li J, Girotti P1, Königsrainer I, et al. (2014) Indications and limits for associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Lessons Learned from 15 cases at a single centre. Z Gastroenterol 52: 35–42.
- Kremer M, Manzini G, Hristov B, Polychronidis G, Mokry T, et al. (2015) Impact of Neoadjuvant chemotherapy on hypertrophy of the future liver remnant after associating liver partition and portal vein ligation for staged hepatectomy. J Am Coll Surg 221: 717– 728.
- Truant S, Scatton O, Dokmak S, Regimbeau JM4, Lucidi V, et al. (2015) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): impact of the inter-stages course on morbi-mortality and implications for management. Eur J Surg Oncol 41: 674–682.
- Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of surgery 240: 205–213.
- Nagino M, Kamiya J, Nishio H , Ebata T, Arai T, et al. (2006) Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg 243: 364-372.
- Tanaka K, Shimada H, Matsuo K, Ueda M, Endo I, et al. (2007) Remnant liver regeneration after two-stage hepatectomy for multiple bilobar colorectal metastases. Eur J Surg Oncol 33: 329-335.
- Knoefel WT, Gabor I, Rehders A, Alexander A, Krausch M, et al. (2013) In situ liver transection with portal vein ligation for rapid growth of the future liver remnant in two-stage liver resection. Br J Surg 100: 388-394.
- Lang, H (2016): ALPPS for colorectal liver metastases. J Gastrointest Surg 21: 190-192.
- Bertens KA, Hawel J, Lung K, Buac S, Pineda-Solis K et al. (2015) ALPPS: challenging the concept of unresectability--a systematic review. Int J Surg 13: 280-287.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences