Hypovitaminosis D and Low Bone Mineral Density in Inflammatory Bowel Disease Patients
Gherardo Tapete, Veronica Almerigogna, Andrea Cozzi, Martina Giannotta, Stefano Milani, Monica Milla and Silvia Biagini
DOI10.4172/2472-1891.100013
Gherardo Tapete*, Veronica Almerigogna, Andrea Cozzi, Martina Giannotta, Stefano Milani, Monica Milla and Silvia Biagin
AOU Careggi, Regional Referral Center of Inflammatory Bowel Disease-Gastroenterology 1 Division, Florence, Italy.
- *Corresponding Author:
- Gherardo Tapete
AOU Careggi, Regional Referral Center of Inflammatory Bowel Disease - Gastroenterology 1 Division
Florence, Italy
Tel: + 39 055 7946828
Fax: +39 0557946805
E-mail: gherardo.tapete@gmail.com
Received date: September 15, 2015 Accepted date: January 05 2016 Published date: January 12, 2016
Citation: Tapete G, Almerigogna V, Cozzi A, et al. Hypovitaminosis D and Low Bone Mineral Density in Inflammatory Bowel Disease Patients. Int J Dig Dis. 2016, 2:1. doi:10.4172/2472-1891.100013
Abstract
Background: Increasing evidences suggest that hypovitaminosis D can play an important role in immuno-mediated diseases, such as Inflammatory Bowel Diseases (IBD). The hypovitaminosis D is an established risk factor for the development of osteopenia, osteoporosis and pathological fractures. Studies have reported a correlation between hypovitaminosis D, disease history and clinical features in Crohn's Disease (CD) and Ulcerative Colitis (UC). The aim of this study is to evaluate the vitamin D serum levels and the prevalence of bone mineral density (BMD) alterations in a population of Italian IBD patients and to correlate the prevalence of hypovitaminosis D with disease history and clinical features.
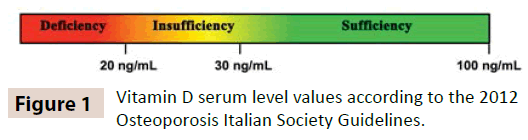
Method: Between October 2013 and November 2014 we enrolled patients from our center that were affected by UC or CD. Exclusion criteria were age below 18 and over 60, concomitant vitamin D replacement therapy and concomitant gastrointestinal or endocrinological diseases which may alter vitamin D metabolism. All patients underwent 25-OH-vitamin D, ESR, C-reactive protein (CRP), PTH, serum calcium and phosphorus, β-CTX, alkaline phosphatase (bone isoenzyme) plasma assay and bone mass density (BMD) evaluation by lumbar and femoral dual-energy X-ray absorptiometry (DXA) scan. Both measurements were made at the same time, during the autumn and winter months. Following 2012 Osteoporosis Italian Society Guidelines, we defined as hypovitaminosis D plasmatic values <30 ng/mL, vitamin D levels were considered as insufficient if between 20 and 30 ng/ mL and deficient if <20 ng/mL. We collected data regarding patients’ life habits and clinical history, disease course and disease clinical activity at enrollment. For BMD evaluation T-score and/or Z-score were calculated for each patient at lumbar (L1-L4) and femoral neck level, and the diagnosis of osteopenia or osteoporosis was made according to international guidelines.
Results: We enrolled 88 patients (62 CD, 26 UC); median age at enrollment was 42 years for CD and 43 years for UC. Mean Body Mass Index (BMI) was 22.6 in CD and 23.7 in UC patients. Age at diagnosis was 29.8 years for CD and 33.5 years for UC, with mean disease duration of 12.8 years for CD and 9.1 years for UC.Hypovitaminosis D was observed in 84.1% of the patients. Of these, 31.8% had insufficient vitamin D levels, whereas 57.3% deficient. Mean vitamin D level was 20.4 ng/mL, but there was no difference with respect to sex or disease type. Indeed, there was no correlation between hypovitaminosis D and disease duration or patients age at diagnosis. A statistically significant correlation was found between hypovitaminosis D and history of steroid-dependancy (p=0.03), need of therapy with anti- TNF-α drugs (p=0.01) and cigarette smoke habit in CD patients (p=0.01). In CD patients we also found a correlation, at the limit of statistical significance (p=0.05), between hypovitaminosis D, high CRP values and HarveyBradshaw Index (HBI) at enrollment.70 patients underwent the lumbar DXA analysis, 67 the femoral DXA. Lumbar BMD was found to be below the normal range in 37.1% of the patients, suggesting that 24.2% and 12.9% were affected by osteopenia or osteoporosis, irrespective of sex and disease type (CD or UC). Similarly, femoral BMD was below the normal range for age in 43.3% of the patients. This figure is consistent with osteopenia or osteoporosis in 34.3% and 9%, irrespective of sex and disease type and femoral Z-score that was found significantly lower in CD than UC patients (p=0.03). Reduced BMD correlated with lower BMI and hypovitaminosis D.
Conclusion: In our study we found a high prevalence of hypovitaminosis D in an IBD population irrespective of patients' sex, type and duration of disease. Our data show a strong correlation between hypovitaminosis D and a more aggressive disease course in terms of history of steroiddependancy, need of therapy with anti TNF-α drugs and smoke habit in CD patients. Hypovitaminosis D may play a crucial role in causing a more severe clinical behavior of IBD. Alteration of bone metabolism is a concern in IBD patients. We observed a high prevalence of BMD alterations in both men and women affected by UC and CD, even if of young age and with a short disease duration, irrespective of the type of IBD. Such patients may be prescribed lumbar and femoral, especially in cases of hypovitaminosis D and low BMI. This would allow an early diagnosis of BMD alterations, to start specific therapy and to prevent further complications.
Keywords
Inflammatory bowel disease; Ulcerative colitis; Crohn’s disease; Vitamin D; Bone mineral density; Osteoporosis
Abbreviations
BALP: Alkaline Phosphatase Bone Isoenzyme; β-CTX: C-Terminal Crosslinked Telopeptide of Type I Collagen; BMD: Bone Mineral Density; BMI: Body Mass Index; CD: Crohn’s Disease; CRP: C-Reactive Protein; DXA: Dual-Energy X-Ray Absorptiometry; EIMs: Extraintestinal Manifestations; ESR: Erythrocyte Sedimentation Rate; HBI: Harvey Bradshaw Index; IBD: Inflammatory Bowel Disease; SIOMMMS: Italian Society of Osteoporosis, Mineral Metabolism and Skeletal Diseases; TNF-α: Tumor Necrosis Factor-α; UC: Ulcerative Colitis.
Introduction
Inflammatory Bowel Disease (IBD), are a group of diseases that comprises the Crohn’s disease (CD) and the Ulcerative Colitis (UC). These are inflammatory diseases of the gastrointestinal tract with a chronic and relapsing course and can cause a lot of extraintestinal manifestations [1-3]. Last decades saw an increased occurrence of CD and UC, with earlier age of onset. The etiology of these diseases is still unknown and their pathogenesis is very complex, including genetic and environmental risk factors, the role of the intestinal microbiota and an altered immune response [1,4,5].
These diseases affect strongly a range of young-adult population in active working and reproductive age [1, 3,6]. Although they do not cause a reduction of life expectancy, these diseases have a detrimental effect not only on the health of individual patients but also on the entire society, causing an increase of direct and indirect costs for the medical care.
In this pathogenetic contest, not fully understood, interest has arisen in the role of vitamin D. Changes in serum levels of vitamin D are very common in the general population, especially in the Northern European countries. Given the lower exposure to sunlight at these latitudes, the skin synthesizes a lower share of vitamin D. Nevertheless, many studies have shown a high incidence of hypovitaminosis D also in Mediterranean countries such as Italy, Greece and Spain. The dietary intake of vitamin D in Italy is limited and it is estimated that this contributes about 20% of the need. Animal fat content in foods like fish is the major dietary source of vitamin D, but this is a minor nutrient contribution to the diet in Western coutries. [7, 8] Historically, the study of the functions of this fat-soluble vitamin has concentrated on its role in the maintenance of calcium and phosphate metabolism. However, the research focus is shifting on the other functions of vitamin D, especially on its immunoregulatory activity and control of the intestinal barrier function. Studies proved that vitamin D has a direct immunoregulatory action which involves both the innate and adaptive immunity. Several cells of the immune system, such as the dendritic cells, macrophages and lymphocytes, not only have receptors for vitamin D, but also can directly synthesize the biologically active form of this vitamin – calcitriol - from the inactive form, the 25-OH-vitamin D. As a consequence, these cells can develop a tight autocrine and paracrine control of their antiinflammatory activity [9-13]. The lack of this immunoregulatory activity exerted by the vitamin D is increasingly researched in pathogenesis studies of many immune-mediated inflammatory diseases such as multiple sclerosis, type 1 diabetes, rheumatoid arthritis, alopecia and IBD [9,14].
Low serum levels of vitamin D are commonly observed in patients affected by IBD. This would suggest that such low levels would be the cause of, not only, an alteration of bone metabolism in patients, that are more susceptible to osteopenia and osteoporosis and pathological fractures, but also of some pathogenetic processes critical to the establishment and perpetuation of the anomalous immune response underlying these diseases. Therefore, the study of the role of vitamin D in IBD may be a new and innovative approach to explain the pathogenesis of IBD, and may have important therapeutic implications on the clinical approach towards these diseases.
The connection between the serum levels of vitamin D and the reduced BMD in IBD patients is another important aspect that this kind of studies might highlight. This would allow a better risk assessment of pathological fractures due to an altered metabolism of vitamin D. Furthermore, understanding the correlation between the vitamin D levels, bone metabolism and the disease history would be relevant for example, from the farmacological point of view, to tune the steroid therapy. The cascade benefit would be the prevention of possible complications which, otherwise, could even worsen the quality of life at another level than IBD itself, especially in patients with a long history of disease.
Aim of the Study
This prospective experimental study was to assess the condition of the bone metabolism and serum levels of vitamin D in IBD patients, in order to find possible correlation between the condition of hypovitaminosis D and the disease characteristics.
Materials and Method
Patient selection
Between October 2013 and November 2014, we enrolled patients with Crohn's Disease (CD) or Ulcerative Colitis (UC) that were examinated at the Regional Reference Center for Inflammatory Bowel Disease, SOD 1 Gastroenterology of the University Hospital of Careggi, in Florence, Italy. In order to avoid substantial differences between the analysis of vitamin D values and the results of the DXA measurements, all patients underwent both measurements at the same time, in autumn or winter months; patients who were enrolled during spring or summer of 2014 were asked to come again in October and November 2014 to our department for a second clinical examination and to perform the blood and urine assays and to perform the DXA measurements.
All patients were diagnosed with IBD according to the clinical, endoscopic and histological criteria defined by the current national and international guidelines. We excluded from the study patients with age <18 years or >60 years, those who were receiving vitamin D supplementation and patients with intestinal or endocrinological diseases which could have interfered with the metabolism of vitamin D. This is the case, for instance, of patients affected by celiac disease and other acute or chronic enteropathies, rickets, advanced liver or kidney diseases, primary and secondary thyroid diseases, parathyroid diseases. All patients signed informed consent to the study.
Data collection
We collected data on the individual characteristics of the patients, their habits and characteristics of the disease. The patients’ medical records and a questionnaire distributed during the examination or by telephone interview were used as source of data.
With regard to the individual characteristics we collected information about age, sex and body mass index (BMI). The latter was calculated as weight (Kg) divided by height squared (m2) according to standards of the World Health Organization (BMI < 18.49 is considered as “underweight”, 18.5 to 24.99 as “normal weight”, 25 to 29.99“overweight”, 30 to 34.99 “obese class I”, 35 to 39.99 “obese class II”, > 40 “obese class III”). We also investigated the smoking habits. To this purpose we considered “smoker” any active smoker or patient with an abstinence period <6 months and “former smokers” patients with >6 months of abstinence. We assessed the consumption of alcoholic beverages, by standardizing the values obtained with the unit of measurement “Alcoholic Unit”, the consumption of beverages containing caffeine (if >3/day), the holding of regular physical activity (if > 3 hours/week) and the use of oral contraceptives. The Alcoholic Unit used corresponds to 1 glass of wine of 125 mL, or 330 mL of beer, or 30-40 mL of super alcoholic beverage. For men it was accepted a quantity of alcohol < 2 alcoholic unit as normal daily consumption of alcohol, while < 1 for women. To better assess the data relating to the structure of the bone metabolism, of the enrolled patients we investigated history of previous bone fractures, history of osteoporosis (including that of the patients’ families) and any history of specific therapy for osteoporosis, both if undertaken in the past or ongoing at the time of examination.
To characterize the disease, of each patient we recorded: age at the onset of the intestinal disease; disease duration; need of steroids before 25 years of age; history of steroiddependence, according to the current definition of the European Guidelines; need of treatment with anti-TNF-α drugs (infliximab, adalimumab); patient’s medical history of intestinal surgery, with particular attention to previous bowel resections and/or packaging of permanent stoma; presence of any extra-intestinal manifestations of IBD with particular attention to the joint diseases, dermatological or eye diseases.
Further elements investigated at the time of enrollment included: clinical activity of disease by calculating the Harvey-Bradshaw Index (HBI) for CD patients and the Mayo Score for those suffering from CU; extent of disease according to the classification of Montreal; current treatment for the intestinal disease.
Laboratory tests
All the patients enrolled were required to undertake blood sampling for the evaluation of the laboratory tests regarding the status of vitamin D metabolism and homeostasis of calcium and phosphate, in addition to the inflammatory markers. We assayed the 25-OH-vitamin D, PTH, serum calcium and phosphorus, β-CTX, alkaline phosphatase bone isoenzyme (BALP), ESR and CRP. The dosage of urinary calcium and phosphaturia were carried out on urine sample from 24-hour collection.
For the purposes of calculation, we used the limits set by SIOMMMS (Italian Society of Osteoporosis, Mineral Metabolism and Skeletal Diseases) in 2012 [15] to define and characterize the condition of hypovitaminosis D. Values between 20-30 ng/mL were classified “insuffiency” and values <20 ng/m “deficiency” (Figure 1).
The 25-OH-D levels were measured by radioimmunoassay (25-Hydroxyvitamin D 125 I RIA Kit, DiaSorin, intra- and interassay CV=11). Biologically active intact PTH was measured by immunoradiometric assay (N-tact® PTH SP Irma Kit, DiaSorin, intra-assay CV=3.6%, interassay CV=4.9%). The 25-OH-D assays were performed from the October 2013 to April 2014 and from the end of September 2014 to November 2014, in order to avoid the effects of the summer sunlight exposure on vitamin D levels.
ESR was measured using the Westergren method, and expressed in mm/hour. An ESR of <15 mm/hour was considered to be normal for males and an ESR of <20 mm/hour was considered to be normal for females. Serum CRP concentrations were measured using a nephelometric immunoassay, and expressed in mg/dL. A CRP of <0.5 mg/dL was considered to be normal.
Blood calcium concentrations were measured within a few minutes of sampling with an ICA Kit (McLendon Clinical Laboratories, Chapel Hill, NC, USA). The normal range considered was 8.5-10.2 mg/dL.
Serum levels of bone-specific alkaline phosphatase (BALP) activity were assayed with a Metra® BAP EIA kit (Quidel Corporation, San Diego, CA, USA). The test utilizes a monoclonal anti-BALP antibody coated on the plate to capture BALP in the sample; the enzyme activity of the captured BALP is detected through the conversion pNPP substrate into PNP. Cross-reactivity of the antibody against the liver form of alkaline phosphatase is low (3–8%). Maximum intra- and inter-assay CVs were 5.8 and 7.6%, respectively, and the detection limit was 0.7 U/L.
C-terminal crosslinked telopeptide of type I collagen (Cross Laps, also known as β-CTX) assays were performed with a Serum CrossLaps® ELISA kit (Immunodiagnostic Systems). Maximum intra- and inter-assay CVs were 3.0 and 10.9%, respectively, and the detection limit was 0.020 ng/mL.
Lumbar and femoral D.X.A
Lumbar and femoral DXA were undertaken for all the patients, with T-score and/or Z-score calculation. We chose not to repeat the examination for those patients who had already performed it in the previous 18 months to limit the exposure to ionizing radiations and to save resources.
The Dual Energy X-ray Absorptiometry analysis were all performed using the Hologic Delphy A device avaible at the Orthopedic Trauma Center of Florence. The T-score and Z-score population of reference used was the BMDCS/Hologic. In order to avoid substantial differences between the analysis of the values of vitamin D and the results of the DXA measurements, both measurements were made at the same time, during the autumn and winter months. Patients enrolled during the spring and summer months of 2014 were asked to come again in October and November 2014 for a second clinical examination and to perform blood and urine tests and to perform the DXA measurement.
BMD was measured by the DXA device at the spine (L1-L4) and the neck of the left proximal femur. The BMD was determined according to the 1994 WHO criteria. For postmenopausal female patients and males older than 50 yrs. a T-score between -1 and -2.5 SD below the mean value for the young adult population was defined as “osteopenia”, and a T-score lower than 2.5 SD below the population mean was defined as “osteoporosis”. The Z-score calculation was used for premenopausal women and for male patients younger than 50 yrs: a Z-score greater than -2.0 SD was defined as “within the normal range for age”, and a Z-score of -2.0 SD or lower was defined as “below the expected range for age”. For these patients, the DXA response reported a framework of patient results within the WHO classification.
Data analysis
We analyzed the collected data using GraphPad Prism 5.0 software. Groups of dichotomous data were compared according to a contingency table by checking the working hypothesis by the nonparametric Fisher test (or Fisher-Yates test, Fisher- Irwin test, χ2;). We also checked whether there was correlation between the data groups by means of linear regression test between the means of the experimental groups using the “T test”.
A value of p<0.05 was considered as statistically significant. To exclude or control confounding variables we carried out our analysis both through experimental design and before the data gathering, and through statistical analysis after the data gathering process. In the first case, biological samples and radiological analysis were performed by the same operator, using the same equipment, so that the bias due to the use of different instruments was reduced. Furthermore, blood samples for the analysis of the vitamin D levels were collected in autumn and winter periods to avoid the bias due to solar light exposure.
To actively exclude or control confounding variables we restricted the sample to patients with age over 18 and below 60 yrs, not assuming concomitant vitamin D replacement therapy and not affected by gastrointestinal or endocrinological diseases which may have altered vitamin D metabolism.
Finally we focused on two of the possible confounding factors: gender and type of disease, the latter being Crohn’s Disease or Ulcerative Colitis. We produced these stratifications and used Mantel-Haenszel (M-H) estimator to provide an adjusted result according to the strata. There was no difference between the raw result and the adjusted one produced by stratification.
Results
Characteristics of population
We enrolled 88 patients of Caucasian ethnicity, with almost equal distribution by sex (45 M; 43 F), of which 62 with CD (31 M, 31 F) and 26 with UC (14 M, 12 F). The mean age at the time of enrollment was 42.3 years (range 18-60 yrs) with no significant difference between CD (mean 42.1 yrs.; range 18-60 yrs.) and UC patients (mean 42.6 yrs; range 21-59 yrs) (Table 1).
| CROHN’SDISEASE | ULCERATIVECOLITIS | |
|---|---|---|
| Mean Age(range) | 42.1 yrs(18-60) | 42.6yrs(21-59) |
| Mean BMI(range) | 22.6(16.9-34) | 23.7(17.4-30.7) |
| Smokers | 48.4% (30/62) | 15.4% (4/26) |
| Formersmokers | 25.8% (16/62) | 42.3% (11/26) |
| Physicalactivity | 25.6% (14/62) | 42.3 (11/26) |
Table 1: Characteristics of population.
BMI calculation showed values generally within the normal range with an average of 22.9 (range 16.9-34), slightly lower in women (mean 22.4, range 16.9-34) than men (mean 23.4, range 18.6- 30.7). In particular, we found BMI <18.5 (underweight) in only 4/88 (4.5%) patients. These were 2 women CD and 2 UC patients. In patients with CD the mean BMI was 22.6 (range 16.9-34), 22.4 for women (range 16.9-34) and 22.8 for men (range 18.6-29). In patients with UC, the mean BMI was 23.7 (range 17.4-30.7), 22.3 for women (range 17.4-29.7) and 24.9 for men (range 20-30.7).
Smoking habits were evaluated in the subgroup of patients with CD. 48.4% (30/62) of the patients were active smokers (13 F, 17 M) while 25.8% (16/62) were former smokers (8 F, 8 M).
In our series, only 28.4% (25/88) of the patients held regular physical activity, in particular only 16.3% (7/43) of the female patients and 40% (18/40) of the men, with a statistically significant difference between the sexes (p=0.03). The prevalence of regular physical activity performance was 25.6% (14/62) of the patients with CD and 42.3% (11/26) of the patients with UC, with no statistically significant difference between the two diseases (p=0.1).
Disease’s characteristics
In general the average age at the onset of the disease was 30.9 years (range 10-56 yrs), lower in the CD (average 29.8 yrs, range 15-56) compared to the UC (average 33.5 yrs, range 10-49). The average duration of the disease was 11.8 years (range 1-36 yrs), higher for CD patients (mean 12.9 yrs, range 2-36 yrs) compared to those with UC (mean 9.1 yrs, range 1-24 yrs).
The distribution of the patients regarding the location and extent of the disease (following the Montreal classification) was: for the CD, 25 patients with localization L1, 5 patients with localization L2, 31 patients with localization L3 and 1 patient with localization L3+L4; for UC 1 patient with extension E1, 10 patients with extension E2, 15 patients with extension E3.
From the pharmacological point of view, we found a history of steroid dependence in 25% (22/88) of the patients, particularly in 24.2% (15/62) of the patients with CD and in 26.9% (7/26) of the patients with UC. The need to resort to therapy with anti TNF-α drugs occurred in 37.5% (33/88) of the cases, in particular in 43.5% (27/62) of the patients with CD and 19.2% (5/26) of the patients suffering from UC. The ongoing treatment at the time of enrollment included the use of thiopurine in 27 patients (CD 17, UC 10), mesalazine in 26 patients (CD 15, UC 11), anti TNF-α drugs in 24 patients (CD 22, UC 2), sulfasalazine in 7 patients (CD 6, UC 1) and systemic steroids in 2 patients (CD 1, UC 1). Two patients (1 with CD, 1 with UC who underwent colectomy with packaging ileal pouch-anal anastomosis) were not receiving any specific treatment for the intestinal disease at the time of enrollment.
The evaluation of the surgical history showed that 40.9% (36/88) of the patients had had intestinal resection surgery. In particular, the need to resort to the surgery occurred in 11.5% (3/26) of the patients with UC and in 53.2% (33/62) of the patients with CD. Among the patients operated for Crohn's disease the surgery was ileocecal resection or ileocolonic in 22 patients, ileal resection in 8 patients, colonic resection in 2 patients and jejunal resection in 1 patient. Of the total of the patients undergoing surgery 7/36 (19.4%), 1 with UC and 6 with CD were carriers of definitive ostomy.
In our study we found a prevalence of 25% of extra-intestinal manifestations with similar rates between the CD (25.8%) and UC (26.9%) (Table 2).
| CROHN’SDISEASE | ULCERATIVECOLITIS | |
|---|---|---|
| Age at the onset(yrs) | 29.8(15-56) | 33.5(10-49) |
| Average duration of disease(yrs) | 12.9(2-36) | 9.1(1-24) |
| Steroid-dependency | 24.2% | 26.9% |
| Need for anti-TNF-adrugs | 43.5%(27/62) | 19.2%(5/26) |
| Previous Intestinalresection | 53.2%(33/62) | 11.5%(3/26) |
| Permanentostomy | 6 | 1 |
| EIMs | 25.8% | 26.9% |
Table 2: Disease’s characteristics.
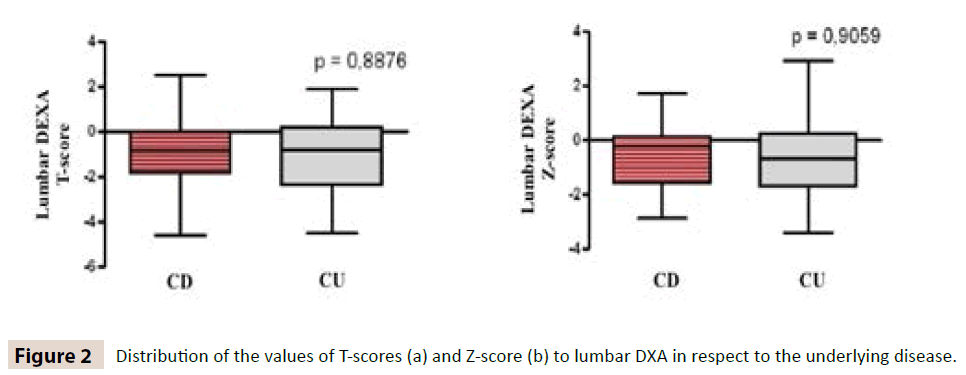
D.X.A
Of the 88 patients enrolled, 70 performed the lumbar DXA and 67 the femoral DXA, with calculation of the T-score and/or Z-score where indicated. The values of bone densitometry at the lumbar level were below the normal range in 37.1% (26/70) of the patients; in particular in 24.2% (17/70) of the cases the alteration was compatible with a framework of osteopenia and in 12.9% (9/70) with osteoporosis. Any alteration of the values of the lumbar DXA was present in 42.1% (16/38) of the female patients and in 31.3% (10/32) of the male patients. The prevalence of lumbar osteoporosis was 15.8% (6/38) in women and 9.4% (3/32) in men. The prevalence of osteopenia and osteoporosis in patients with CD was, respectively, 25.6% (12/47) and 10.6% (5/47), while for the UC we found a prevalence of 24.3% (5/23) for osteopenia and 17.4% (4/23) for osteoporosis.
The BMD values of femoral neck were reduced in 43.3% (29/67) of the patients; in particular, in 34.3% (23/67) of the cases the alteration was compatible with osteopenia and 9% (6/67) with osteoporosis. Any alteration of the femoral DXA values was found in 54.1% (20/37) of the female patients and in 30% (9/30) of the male patients. The prevalence of femoral osteoporosis was of 13.5% (5/37) in women and 3.3% (1/30) in men. In CD patients, instead, the prevalence of osteopenia and osteoporosis was respectively 34.8% (16/46) and 10.9% (5/46), while in the UC we found a prevalence of 33.3% (7/21) of osteopenia and 4.7% (1/21) of osteoporosis (Table 3).
| CROHN’SDISEASE | ULCERATIVECOLITIS | |||
|---|---|---|---|---|
| LUMBAR DXA | FEMORAL DXA | LUMBAR DXA | FEMORAL DXA | |
| Normal | 63.8% | 54.3% | 60.9% | 62% |
| Osteopenia | 25.5% | 34.8% | 21.7% | 33.3% |
| Osteoporosis | 10.6% | 10.9% | 17.4% | 4.7% |
Table 3: D.X.A.
We have, also, divided the patients into 3 groups according to age (15-30 yrs, 31-50 yrs, >50 yrs), and we got these results: for patients with CU, in the group between 15-30 yrs, 33,3% (1/3) of male patients showed osteopenia, while 100% (02/02) of women in the same age had normal BMD; in the group between 30-50 yrs, 33.3% (2/6) of males showed osteoporosis, while among women 28.57% (2/7) osteopenia and 14.28% (1/7) osteoporosis; above 50 years of age, 100% (2/2) of women with CU had normal levels of BMD, while 66.6% (2/3) of males showed osteopenia and 33.3% (1/3) osteoporosis.
As it regards the lumbar DXA of patients with CD, in the range 15-30 yrs, 16.66% (1/5) of males and 50% of women (1/2) had osteopenia; between 31-50 yrs, 10% (1/10) of males showed a framework of osteopenia, while among women 28.57% (4/14) had osteopenia and 7,14% (1/14) osteoporosis; over age of 50 yrs, 25% (1/4) of males and 27.26% (3/11) women had a framework of osteopenia, while 36,37% (4/11) of the women had osteoporosis (Table 4).
| RCU LUMBAR DXA | ||||||
|---|---|---|---|---|---|---|
| N° | Healthy (%) | Osteopenic (%) | Osteoporotic (%) | Lumbar T-score | Lumbar Z-score | |
| Male ≤ 30_yrs (range 18–30) | 3 | 66,7% | 33,3% | 0% | -0,75 ± 1,05 | -0,75 ± 1,05 |
| Male 31–50_yrs | 6 | 66,7% | 0% | 33,3% | -1,6 ± 1,8 | -1,6 ± 1,8 |
| Male >50_y (range 51–60) | 3 | 0% | 66,7% | 33,3% | -2,65 ± 0,35 | -1,95 ± 0,45 |
| Female ≤ 30_yrs (range 17–30) | 2 | 100% | 0% | 0% | 0,45 ± 0,45 | 0,45 ± 0,25 |
| Female 31–50_yrs | 7 | 57,15% | 28,57% | 14,28% | -0,6 ± 2,5 | 0,25 ± 2,65 |
| Female >50_yrs(range 51–60%) | 2 | 100% | 0% | 0% | -0,1 ± 0,5 | 0,4 ± 1,0 |
| CD LUMBAR DXA | ||||||
| N° | Healthy (%) | Osteopenic (%) | Osteoporotic (%) | Lumbar T-score | Lumbar Z-score | |
| Male ≤ 30_yrs (range 18–30) | 6 | 66,7% | 33,3% | 0% | -0,7 ± 1,4 | -0,65 ± 1,45 |
| Male 31–50_yrs | 10 | 90% | 10% | 0% | -0,6 ± 1,4 | -0,55 ± 1,35 |
| Male >50_yrs (range 51–60) | 4 | 75% | 25% | 0% | -0,65 ± 1,55 | -0,3 ± 1,7 |
| Female ≤ 30_yrs (range 17–30) | 2 | 50% | 50% | 0% | -1,005 ± 0,995 | -0,95 ± 0,95 |
| Female 31–50_yrs | 14 | 64,29% | 28,57% | 7,14% | -1,25 ± 1,75 | -0,95 ± 1,95 |
| Female >50_yrs (range 51–60%) | 11 | 36,37% | 27,26% | 36,37% | -1,05 ± 3,55 | -0,55 ± 2,25 |
Table 4: Lumbar DXA of patients with CD.
At femoral level, in patients with CU, we found: in the 15-30 yrs group, osteopenia in 33.33% (1/3) of males; in the group between 31-50 yrs, in 60% (3/5) of males and 50% (3/6) of women had osteopenia, and osteoporosis in 20% (1/5) of males; over 50 years, no patient with CU showed reduction in BMD.
Among the CD patients, the femoral DXA showed: between 15 and 30 yrs, 16.67% (1/6) of male with osteopenia, while 50% (1/2) of women with osteoporosis; in the group between 15- 30 yrs, 10% (1/10) of males and 53.33% (8/15) had osteopenia, while 20% (3/15) of women osteoporosis; over 50 yrs, 50% of males (2/4) and 44.44% (4/9) of the women had a framework of osteopenia and 11.2% (1/9) of women osteoporosis (Table 5).
| RCU FEMORAL DXA | |||||||
|---|---|---|---|---|---|---|---|
| N° | Healthy (%) | Osteopenic (%) | Osteoporotic (%) | Femoral T-score | Femoral Z-score | ||
| Male ≤ 30_yrs (range 18–30) | 3 | 66,7% | 33,3% | 0% | 0.8 | 0.9 | |
| Male 31–50_yrs | 5 | 20% | 60% | 20% | -0.5 | -0.3 | |
| Male > 50_yrs (range 51–60) | 2 | 100% | 0% | 0% | -0.6 | -0.2 | |
| Female ≤ 30_yrs (range 17–30) | 2 | 100% | 0% | 0% | -0.5 | -0,7 ± 0.1 | |
| Female 31–50_y | 6 | 50% | 50% | 0% | 1.1 | -0,4 ± 1.6 | |
| Female >50_yrs (range 51–60%) | 3 | 100% | 0% | 0% | 0.7 | 0.55 ± 0.85 | |
| CD FEMORAL DXA | |||||||
| N° | Healthy (%) | Osteopenic (%) | Osteoporotic (%) | Femoral T-score | Femoral Z-score | ||
| Male ≤ 30_yrs (range 18–30) | 6 | 83,33% | 16,67% | 0% | 0.6 | 0.6 | |
| Male 31–50_yrs | 10 | 90% | 10% | 0% | 0.5 | 0.3 | |
| Male >50_yrs (range 51–60) | 4 | 50% | 50% | 0% | -0.4 | 0.5 | |
| Female ≤ 30_yrs (range 17–30) | 2 | 50% | 0% | 50% | -0.8 | -0.8 | |
| Female 31–50_yrs | 15 | 26,67% | 53,33% | 20% | 0 | -1,4 ± 2 | |
| Female >50_yrs (range 51–60%) | 9 | 44,4% | 44,4% | 11,2% | 2.2 | 0.1 ± 1.3 | |
Table 5: The femoral DXA among the CD patients.
In our series, we did not find a statistically significant difference regarding the prevalence of osteopenia (p=1 NS) and osteoporosis (p=0.4 NS) at the lumbar level between the two underlying diseases (Figure 2). Similarly we did not find a statistically significant difference regarding the prevalence of osteopenia (p=0.6 NS) or osteoporosis (p=0.6 NS) at the femoral level between the two diseases, but there was a statistically significant difference between CD and UC with regard to the Z- score at the femoral DXA (p=0.03) (Figure 3).
In our series we also found a statistically significant direct correlation between the values of both lumbar and femoral BMD and BMI. Similarly, direct correlation was observed between serum levels of vitamin D and the value of the T-score both in the lumbar (p=0.02) and femoral levels (p=0.02).
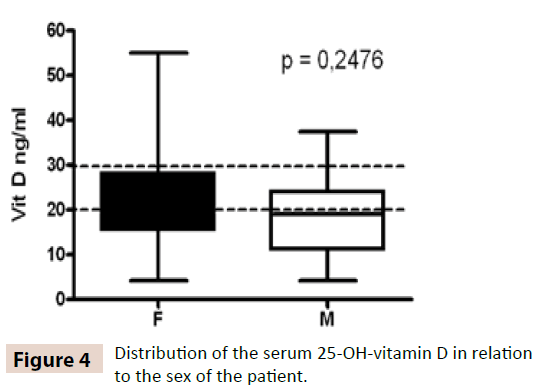
25-OH-Vitamin D levels
The evaluation of serum levels of 25-OH-vitamin D showed a condition of hypovitaminosis D in 84.1% (74/88) of the patients. Most notably 31.8% (28/88) of the patients had values compatible with a state of insufficiency of the vitamin and 52.3% (46/88) had values compatible with a state of shortage. The mean value of the 25-OH-vitamin D was 20.4 ng/mL (range 4.2-68); lower in men (mean 18.3 ng/mL; range 4.2-37.5) than women (mean 22.6 ng/ mL; range 4.2-68). There was no statistically significant difference regarding the prevalence of hypovitaminosis D in relation to the patient sex (p=NS) (Figure 4).
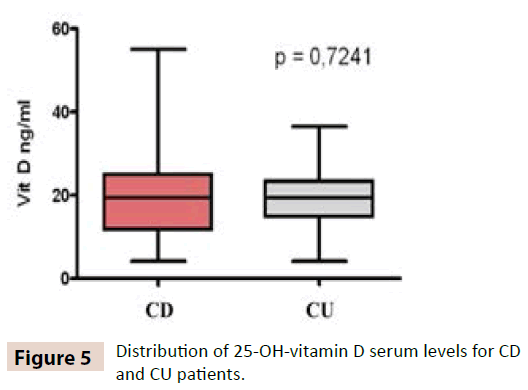
With regard to the CD patients we found a condition of hypovitaminosis D in 83.9% (52/62) of the cases. Most notably 32.3% (20/62) of the patients presented values compatible with a state of insufficiency and 51.6% (32/62) had values compatible with a state of shortage. The mean serum level of 25-OH-vitamin D in these patients was 20.2 ng/mL (range 4.2-55.1); lower in men (mean 18.3 ng/mL; range 4.2-37.5) than women (mean 22 ng/mL; range 4.2-55). Regarding the patients with UC a condition of hypovitaminosis D emerged in 84.6% (22/26) of the cases. Most notably 30.8% (8/26) of the patients presented values compatible with a state of insufficiency of the vitamin and 53.8% (14/26) had values compatible with a state of shortage. The mean serum level of 25-OH-vitamin D in these patients was 20.8 ng/ mL (range 4.2-68); lower in men (mean 18.2 ng/mL; range 4.2- 30.2) than women (mean 23.9 ng/mL; range 10.1-68). There was no statistically significant difference regarding the prevalence of hypovitaminosis D in CD compared to the UC (p=0.7 NS) (Figure 5).
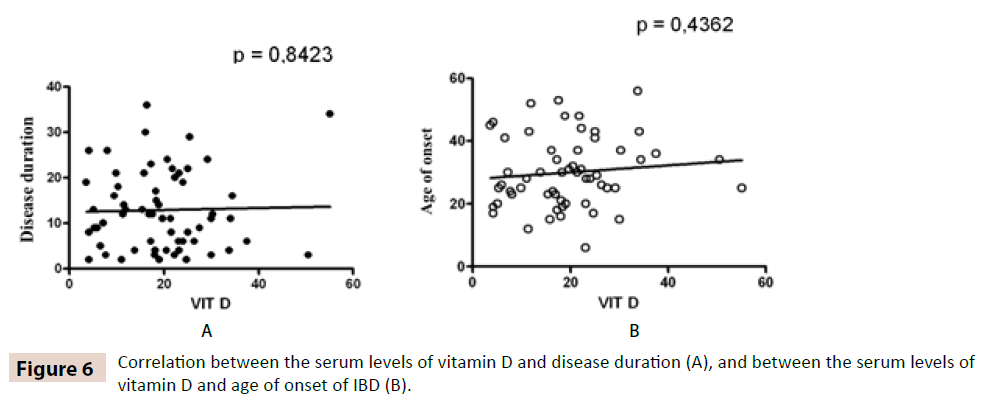
No statistically significant correlation was observed between hypovitaminosis D and disease duration (Figure 6A) or hypovitaminosis D and age of IBD onset (Figure 6B).
With regard to the correlation with the disease activity at baseline at the time of enrollment, in our population we did not find any correlation between hypovitaminosis D in general and alterations of CRP (p=0.2 NS), or between the vitamin D deficiency and alteration of CRP (p=0.4 NS). However, in the subgroup of CD patients hypovitaminosis D occurred in 78.7% (37/47) patients with normal CRP vs. 100% (15/15) of patients with impaired CRP, showing a correlation to the limits of statistical significance (p=0.05). Similarly, in CD patients we did not find any correlation between the general condition of hypovitaminosis D and the Harvey Bradshaw Index (HBI) (p=1 NS), but there was a correlation to the limits of statistical significance between vitamin D deficiency and HBI (p=0.06).
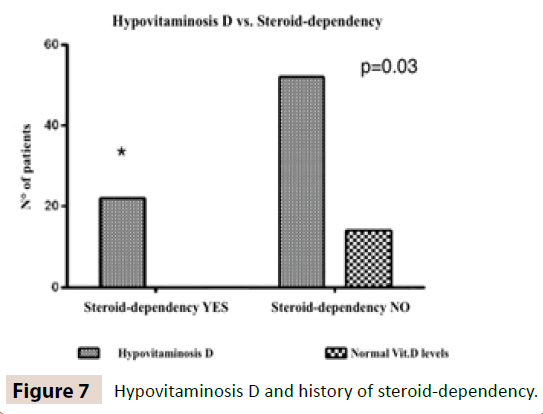
Regarding the correlation between the levels of vitamin D and indirect indices of disease severity, the analysis of the data showed a statistically significant correlation between the hypovitaminosis D and the history of steroid dependency. In our series all the patients (22/22) with a history of steroid-dependent presented hypovitaminosis D vs. 78.8% (52/66) of patients with no history of steroid-dependency (p=0.03) (Figure 7).
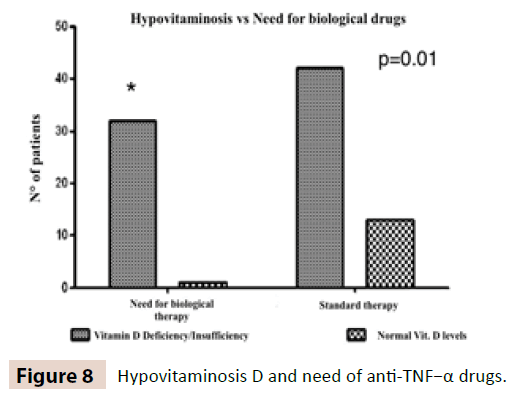
A statistically significant correlation was found between the hypovitaminosis D and the need to resort to the therpy with anti- TNF-α drugs compared to those who have not needed it (97% vs. 76.4%; p=0.01) (Figure 8).
In the subgroup of patients with CD, we have also found a statistically significant correlation between smoking habits and hypovitaminosis D. 29/30 (96.7%) of the active smoker patients presented hypovitaminosis vs. 23/32 (71.9%) of former or nonsmokers (p=0.01).
Instead, we did not found statistically significant correlations between the presence of hypovitaminosis D and the presence of extra-intestinal manifestations (p=0.17 NS), the history of surgery related to inflammatory bowel disease (p=0.8 NS) or the use of steroids before 25 yrs for CD among the patients with age of onset of the illness <25 yrs (p=0.8 NS).
In our population there was not statistically significant correlation between hypovitaminosis D and the habit of not practicing regular physical activity (p=0.7 NS), even in the subgroup of CD patients (p=1 NS). Regarding the correlation between hypovitaminosis D and the localization of disease, in the subgroup of patients with UC no patient with disease limited to the rectum (E1 for Montreal Classification) presented alteration of the values of vitamin D, while 22/25 patients with ulcerative left colitis or extended (E2 or E3 sec. Montreal) had abnormal values of vitamin D; we could notice a trend between the extent of the disease and hypovitaminosis D, although not reaching the limits of statistical significance. In CD no correlation was revealed between hypovitaminosis and ileal localization (p=1 NS).
Finally by the linear correlation test we found a direct correlation between the values of vitamin D and BMI, although without reaching a statistically significant difference neither between hypovitaminosis D and BMI values indicative of body underweight (<18.5) (p=0.1 NS) or between hypovitaminosis D and BMI<25 (p=NS).
Discussion
A high percentage of patients had with low serum levels of vitamin D. Over 30% of the patients had an insufficiency of vitamin D and over 50% showed deficiency. These alterations were observed irrespective of sex and type of intestinal disease. The mean value of 25-OH vitamin D was 20.4 ng/mL. Literature data on the prevalence of hypovitaminosis D in IBD patients are conflicting: a recent meta-analysis which considered more than 20 studies conducted from 1982 to 2013 to assess the prevalence of hypovitaminosis D in patients with IBD, reported percentages between 15 and 95% [16].
However, if we analyze the results obtained from studies on healthy population we find values of hypovitaminosis D in agreement with our results. In particular, a recent study conducted on over 400 healthy adolescents in Tuscany (10-21 years old) showed a prevalence of hypovitaminosis D equal to 82.2%, with 32.3% of insufficiency and 49.9% of deficiency [17]. These results suggest that the high percentage of hypovitaminosis D observed in our series might be primitive and probably gained before the onset of the disease. Only a small part of the alteration would be secondary to the nutritional problems and therapeutic regimes related to these inflammatory bowel diseases.
This hypothesis is supported by the lack of correlation, in our patients, between vitamin D deficiency, age of disease onset and intestinal disease duration. This lack of correlation has been reported in the literature by several authors [18,19] who, among other mechanisms, also suggest a possible important role of vitamin D at the intestinal level that would allow a greater absorption of vitamin D secondary to the beneficial effects of a longer therapy and therefore a better control of the activity of the disease itself. In contrast, other authors have found an inverse correlation between the duration of disease and serum levels of vitamin D, especially in patients with Crohn's disease [20].
The literature highlights an association between hypovitaminosis D and disease activity in IBD expressed in terms of clinical score of disease activity and/or alteration of biochemical markers [21,22]. This correlation appears to be stronger for CD than for UC [23,24]. Our results only partially agree with these studies because we found a correlation to the limits of statistical significance between vitamin D deficiency, abnormal CRP and clinical activity of the disease only in the subgroup of patients with CD. In this sense a limit of our study could be represented by the high prevalence of patients in clinical remission. However, this option needs to be confirmed against a larger series of patients. Conversely, the analysis of the natural history of the patients enrolled in our study showed a clear correlation between hypovitaminosis D and elements which indicate a severe course of illness. Indeed, we found a statistically significant correlation between hypovitaminosis D, history of steroid-dependence and use of anti-TNF-α drugs. Positive correlation between hypovitaminosis D and the use of anti TNF-α drugs has been reported in a study of IBD patient in the northern and central U.S [22].
Another significant correlation was observed in patients with CD, between vitamin D deficiency and smoking habit. This is a factor known to be associated with a more severe course of illness. Our data agree with what has been already reported in the literature by several authors [20,25-27]. The mechanism linking the two aspects has not been clarified yet. On one hand, in animal models, it has been suggested that this would be due to a reduction in the production of endogenous quote of the vitamin D caused by the skin hyperpigmentation because of the exposure to nicotine [28]. On the other hand, it was hypothesized that the nicotinic receptors in the intestinal epithelium could play an important role, even if it is not well defined. At last, other authors proposed the negative influence of smoking on the quality of life of the patient, i.e., as an independent risk factor for the development of hypovitaminosis D [22].
Data in the literature do not agree on the relationship between the ileal involvement in CD and deficiency of vitamin D. Some authors report an association between hypovitaminosis and ileal disease [21,29], while others did not find such correlation [19,25,30]. Our data are consistent with recent studies of Crohn's disease, demonstrating on the contrary a positive trend between hypovitaminosis and the extent of disease in ulcerative colitis. This figure resizes further the genesis secondary to malabsorption of hypovitaminosis in these patients.
The literature contains conflicting data about the relationship between bowel resection surgery, especially in the CD, and hypovitaminosis D. Some studies deny such a correlation [20,25,27], emphasizing the reduction of disease activity following the surgery with consequent beneficial effect on the levels of vitamin D. Other studies, however, indicate a possible correlation with previous surgery of the small intestine. The latter, acting on the site of intestinal absorption of the vitamin D, would cause its malabsorption. Our evidences tend to confirm the hypothesis that there is a significant correlation between these two parameters.
There are few studies in the literature about the relationship between BMI and hypovitaminosis D. These tend to consider the relationship between normal or increased BMI and levels of vitamin D, showing a correlation between high BMI and hypovitaminosis D [19]. In our study, however, we have noticed a correlation between BMI and values of vitamin D, while the reduced values of BMI correlate with an alteration of bone densitometry, as reported by other studies which have addressed this relationship [31].
The literature has not systematically investigated the correlation between vitamin D and the use of corticosteroids. The role of the corticosteroid therapy in patients with IBD has been generally limited to the evaluation of the relationship with alterations in bone densitometry. Few case studies have considered the relationship with the serum level of 25-OH-vitamin D, and in general these studies tend to exclude an inverse correlation between the corticosteroid therapy and the reduction of circulating levels of vitamin D [20]. In our study we revealed a positive correlation between the history of steroid-dependence and reduced levels of vitamin D, while there would be no correlation with the use of corticosteroids under 25 years of age. These last two aspects are not discussed extensively in the literature. Therefore our findings provide a new interesting contribution.
It is known that the IBD are pathologies associated with alterations of the bone metabolism and decreased bone density, so that the Crohn's disease is one of the risk factors for osteoporosis. Literature data report values of osteopenia between 23 and 67% and 7-35% for osteoporosis in patients with IBD. In our study we found an alteration of the BMD values with values of lumbar osteopenia of 24.2% and femoral osteopenia of 34.3%; as it regards the lumbar osteoporosis 12.9% and femoral 9%. The alteration of the DXA does not correlate either with sex or with disease. The absence of correlation with the sex of the patient is discussed in the literature: for some studies there is no difference [32], for other studies, instead, there is a correlation with the male sex, especially for the relief of reduced bone density already at the time of diagnosis [33].
Conclusion
In our study we demonstrated that serum levels of vitamin D were significantly reduced in patients with IBD, without any difference between sexes and the two diseases. We also found shows a strong correlation between hypovitaminosis D and a more aggressive disease course. These observations combine with increasing reports in the literature about widespread hypovitaminosis D even in the healthy population, particularly adolescents, and an increasingly strong correlation of this deficit with the increased prevalence of systemic immune-mediated diseases. Therefore the findings of our study confirm the growing evidence that hypovitaminosis D may play an important role as an independent risk factor in the pathogenesis of IBD and as a possible factor worsening the clinical course of the disease. Only a few studies have evaluated the beneficial effects of vitamin D supplementation on the prevention and treatment of the autoimmune diseases.
Based on these findings it has been suggested to identify and correct the vitamin D insufficiency in IBD patients since the time of diagnosis.
Furthermore, our analysis of the correlation between hypovitaminosis D and densitometric bone alterations in IBD patients has highlighted the presence of a marked reduction in bone density of these subjects, even of young age and with brief history of the disease. This finding is in agreement with most of the international studies. Therefore, it is important to investigate the presence of alterations of bone metabolism in patients with IBD, and in particular in those who have reduced serum levels of vitamin D, in order to prevent the development of complications.
Further research is needed to fully understand the many functions of the vitamin D beyond its traditional role of maintaining homeostasis of calcium, and to identify the mechanisms through which it performs these functions. Such outcomes might clarify the pathogenesis and therapeutic implications of an altered state of the vitamin D on the development and maintenance of many immune-mediated diseases, especially IBD.
References
- Ananthakrishnan AN (2013) Environmental Risk Factors for Inflammatory Bowel Disease. Gastroenterology & Hepatology. 9: 367-374.
- Loftus EV (2004) Jr. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology 126: 1504–1517.
- Cosnes J, Gower-Rousseau C, Seksik P, Cortot A (2011) Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology 140: 1785–1794.
- Abraham C, Cho JH (2009) Inflammatory bowel disease. N Engl J Med 361: 2066–2078.
- Khor B, Gardet A, Xavier RJ Genetics and pathogenesis of inflammatory bowel disease. Nature.
- Carter MJ, Lobo AJ, Travis SP (2004) Guidelines for the management of inflammatory bowel disease in adults. Gut 5: 1-16.
- Holick M.F (2007) Vitamin D deficiency. N. Engl. J. Med 357: 266–281.
- Lamberg-Allardt C (2006) Vitamin D in foods and as supplements. Prog. Biophys. Mol. Biol 92: 33-38.
- Cantorna MT, Mahon BD (2005) D-hormone and the immune system. J Rheumatol 76: 11-20.
- Cantorna MT, Zhu Y, Froicu M, Wittke A (2004) Vitamin D status, 1,25-dihy-droxyvitamin D3, and the immune system. Am J Clin Nutr 80: 1717S–1720S.
- Hewison M (2012) Vitamin D and immune function: an overview. Proc Nutr Soc. 71: 50-61.
- Fritsche J, Mondal K, Ehrnsperger A, Andreesen R, Kreutz M (2003) Regulation of 25- hydroxyvitamin D3-1 alpha-hydroxylase and production of 1 alpha,25- dihydroxyvitamin D3 by human dendritic cells. Blood 102: 3314–3316.
- Liu PT, Stenger S, Li H, Wenzel L, Tan BH et al. (2006) Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science 311: 1770–1773.
- Cantorna MT, Mahon BD (2004) Mounting evidence for vitamin D as an environmental factor affecting autoimmune disease prevalence. Exp Biol Med (Maywood) 229: 1136–1142.
- Adami S, Romagnoli E, Carnevale V, Scillitani A, Giusti A, R (2011) Linee guida su prevenzione e trattamento dell’ipovitaminosi D con colecalciferolo, Reumatismo, 2011; 63: 129-147.
- Mouli, Venigalla Pratap, Ashwin N A (2014) “Review Article: Vitamin D and Inflammatory Bowel Diseases.” Alimentary pharmacology & therapeutics.
- Vierucci, Francesco (2014) “Prevalence of Hypovitaminosis D and Predictors of Vitamin D Status in Italian Healthy Adolescents.” Italian Journal of Pediatrics.
- Pappa HM, Gordon CM, Saslowsky TM, Zholudev A, Horr B, et al. (2006) Vitamin D status in children and young adults with inflammatory bowel disease. Pediatrics 118: 1950-1961.
- Veit LE, Maranda L, Fong J, Nwosu BU (2014) The Vitamin D Status in Inflammatory Bowel Disease.
- Suibhne TN, Cox G, Healy M, O’Morain C, O’Sullivan M (2012) Vitamin D deficiency in Crohn’s disease: prevalence, risk factors and supplement use in an outpatient setting. J Crohns Colitis 6: 182–188.
- Levin AD, Wadhera V, Leach ST, Woodhead HJ, Lemberg DA, et al. (2011)Vitamin D deficiency in children with inflammatory bowel disease. Dig Dis Sci 56: 830-836.
- Ulitsky A, Ananthakrishnan AN, Naik A (2011) Vitamin D deficiency in patients with inflammatory bowel disease activity and quality of life. JPEN J Parenter Enteral Nutr 35: 308-316.
- Siffledeen J, Siminoski K, Steinhart H, Greenberg G, Fedorak R (2003) The frequency of vitamin D deficiency in adults with Crohn's disease. Can J Gastroenterol 17: 473-478.
- Tajika M, Matsuura A, Nakamura T, Suzuki T, Sawaki A, Kato T et al. (2004). Risk factors for vitamin D deficiency in patients with Crohn's disease. J Gastroenterol 39, 527–533.
- Gilman J, Shanahan F, Cashman KD (2006) Determinants of vitamin D status in adult Crohn’s disease patients, with particular emphasis on supplemental vitamin D use. Eur J Clin Nutr 60: 889-896.
- Lamberg-Allardt CJ, Outila TA, Kärkkäinen MU, Rita HJ, Valsta LM (2001) Vitamin D deficiency and bone health in healthy adults in Finland: could this be a concern in other parts of Europe? J Bone Mineral Res 16: 2066–2073.
- Andersen R, Mølgaard C, Skivgaard LT, Brot C, Cashman KD et al. (2005) Prevalence of hypovitaminosis D in two risk groups in European countries. Eur J Clin Nutr 59: 533–541.
- Palmer, Matthew T, Casey T. Weaver (2013) “Linking Vitamin D Deficiency to Inflammatory Bowel Disease.” Inflammatory bowel diseases 2245–2256.
- Haderslev KV, Jeppesen PB, Sorensen HA, Mortensen PB, Staun M (2003) Vitamin D status and measurements of markers of bone metabolism in patients with small intestinal resection. Gut 52, 653-658.
- Andreassen H, Rix M, Brot C, Eskildsen P (1998) Regulators of calcium homeostasis and bone mineral density in patients with Crohn's disease. Scand J Gastroenterol 33: 1087–1093.
- Atreja, Ashish (2012) “Low Body Mass Index Can Identify Majority of Osteoporotic Inflammatory Bowel Disease Patients Missed by Current Guidelines.” The Scientific World Journal.
- Ediz, Levent, Murat Toprak, Mehmet Fethi Ceylan, Ozgur Kemik (2011) “The Prevalence and Risk Factors of Decreased Bone Mineral Density in Firstly Diagnosed Ulcerative Colitis Patients in the Eastern Region of Turkey.” International Journal of Clinical and Experimental Medicine 157–163. Print.
- Van Schaik FDM, Marc A.M.T. Verhagen, Peter D. S (2008) Journal of Crohn's and Colitis 2: 208-213.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences