Comparison of Insulin Resistance between Nonalcoholic Fatty Liver Disease Patients with and those without Helicobacter pylori Infection
Chen Li-Wei,Chang Liang-Che,Chien Rong-Nan,Chen Chih-Hung,Kuo Sheng-Fong,Chang Jia-Jang,Hu Ching-Chih
DOI10.4172/2472-1891.100011
Chen Li-Wei1*, Chang Liang-Che2, Chien Rong-Nan1, Chen Chih-Hung3, Kuo Sheng-Fong3, Chang Jia-Jang1 and Hu Ching-Chih1
1Department of Gastroenterology and Hepatology, Chang-Gung Memorial Hospital and University at Keelung, Taiwan
2Department of Pathology, Chang-Gung Memorial Hospital and University at Keelung, Taiwan
3Department of Metabolism and Endocrinology, Chang-Gung Memorial Hospital and University at Keelung, Taiwan
- *Corresponding Author:
- Li-Wei Chen
Department of Gastroenterology and Hepatology, Chang-Gung Memorial Hospital and University at Keelung
12F, No 222, Mai-Jin Road, Keelung, Taiwan 20401
Tel: 886-2-24313131
Fax: 886- 3-24335342
E-mail:leiwei@adm.cgmh.org.tw
Received date: September 16, 2015, Accepted date: November 12 2015, Published date: November 19, 2015
Citation: Li-Wei Chen, et al. Comparison of Insulin Resistance between Nonalcoholic Fatty Liver Disease Patients with and those without Helicobacter pylori Infection. Int J Dig Dis. 2015, 1:1. doi:10.4172/2472-1891.100011
Abstract
Aim/background: Insulin resistance [IR] is the key pathophysiological mechanism for nonalcoholic fatty liver disease [NAFLD] and nonalcoholic steatohepatitis [NASH]. Recent studies have disclosed the relationship between Helicobacter pylori (H. pylori) infection and IR. This study aimed to evaluate the differences in IR between NAFLD patients with and those without H. pylori infection.
Patients and method: From January 2011 to December 2012, patients with pathologic proof of NAFLD were included. All patients received a C14 urea breath test for H. pylori infection evaluation. Serum samples were taken for homeostasis model assessment of insulin resistance [HOMA-IR], lipid profile, inflammatory cytokine and adipokine studies. Patients with H. pylori infection received standard triple eradication. Serum samples were then subjected to HOMA-IR three and six months after eradication therapy.
Results: Eleven patients with both NAFLD and H. pylori infection and 18 patients with only NAFLD were included into this study. There were no significant differences between the two groups in demographic, laboratory or histological data. The only difference was mean HDL value. Patients with H. pylori infection had higher mean HDL values than patients without H. pylori infection [50.1 ± 8.8 vs. 38.8 ± 9.7 mg/dL, p=0.004]. The serial values of HOMA-IR from patients with H. pylori infection following H. pylori eradication 0, 3 or 6 months later did not reveal an increasing or decreasing trend following H. pylori eradication treatment. Conclusion: There were no significant differences in HOMA-IR values between NAFLD patients regardless of whether they had H. pylori infection. For patients with NAFLD and H. pylori infection, the HOMA-IR value was not affected by H. pylori eradication treatment.
Keywords
Helicobacter pylori; Insulin resistance; Leptin; Steatohepatitis; Fatty liver
Introduction
Insulin resistance [IR] is the key pathophysiological mechanism for nonalcoholic fatty liver disease [NAFLD] and nonalcoholic steatohepatitis [NASH] [1-4]. Abnormal adipokine (adiponectin, leptin) [5-7] and inflammatory cytokines [8-10] are the “second hit” for the pathogenesis of NASH. The liver may be exposed to the metabolic hepatotoxic byproducts generated by the gut microbiome, including acetaldehyde, ammonia, and phenols. Gut microbiota may be involved in the pathogenesis of NASH [11]. Helicobacter pylori (H. pylori) infection induces chronic inflammation in the human stomach. This inflammatory response may induce local gastritis and systemic immune responses. Recent studies have shown evidence for possible relationships between H. pylori infection, IR [11-13], leptin [14,15] and metabolic syndrome [16-18]. Although IR was reported to be related to both H. pylori infection and NASH, few studies have investigated the influence of H. pylori infection on IR among NASH patients [19-21]. This study aimed to evaluate any difference in homeostasis model assessment of IR [HOMA-IR] values between NAFLD patients with and those without H. pylori infection. For patients with NAFLD and H. pylori infection, the HOMA-IR values were compared before and after H. pylori eradication treatment.
Patients and Method
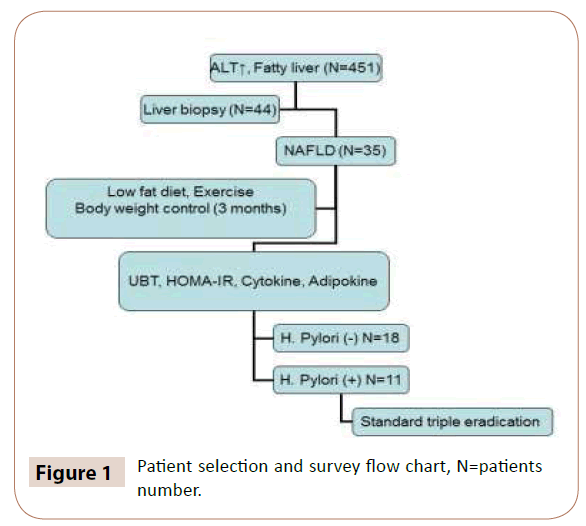
From January 2011 to December 2012, patients with abnormal serum alanine aminotransferase [ALT] values [more than normal upper limit], abdominal ultrasonographic evidence of fatty liver and ultrasound-guided fine needle liver biopsy results characteristic of NASH were included into this study. Exclusion criteria included daily consumption of >10 g alcohol or other compatible volume beer or wine; taking oral hypoglycemia agent; and the presence of chronic inflammation disease such as autoimmune disease or chronic viral hepatitis B or C. A detailed history of alcohol consumption was obtained by two physicians independently and consultation with family members to confirm negligible alcohol consumption [less than 10 g of ethanol per day]. Because exercise, diet control and body weight reduction are important for improving insulin resistance, patients should be asked to take an appropriate exercise and diet control before entering the study. Otherwise, the effect of insulin resistance [HOMA-IR change] could not be attributed to H pylori eradication if the patients also had body weight reduction and adequate exercise. In the first 3 months following inclusion into this study, patients were persuaded to participate in frequent [at least twice per week] appropriate exercises and to maintain a low-fat diet. 3. To prevent interferences in IR test, patients who were diagnosed to have a disease of Diabetic mellius and used antidiabetic agents, such as biguanides [metformin], insulin, thiazolindinediones [pioglitazone] etc, were excluded in the study. All patients received a C14 urea breath test for H. pylori infection evaluation. Serum samples were taken for ALT, cholesterol, triglyceride, fasting glucose/insulin level [for IR evaluation by HOMA-IR], inflammatory cytokines (tumor necrosis factor alfa (TNF-α) and high sensitive C reactive protein (HS-CRP) and adipokine (adiponectin, leptin) studies. Demographic information including age, sex, body weight, body height, and waist circumferences were also collected. Patients with H. pylori infection would receive standard triple eradication with esomeprazole 40 mg, clarithromycin 500 mg and amoxicillin 1 g twice daily for a total of 7 days. For a patient with a history of amoxicillin allergy, the eradication regiments would change amoxicillin into metronidazole. The dose of metronidazole was 500 mg twice per day. After eradication therapy, patients received the same serum tests three and six months later. Follow-up UBT was performed three months after H. pylori eradication (Figure 1).
Homeostasis Model Assessment of Insulin Resistance [HOMA-IR]
The estimate of IR by HOMA score was calculated by the formula: [fasting plasma insulin [mU/L] × fasting plasma glucose [mmol/L]]/22.5. A high HOMA-IR score denotes low insulin sensitivity and IR [22].
Pathologic criteria for NASH
Liver biopsy specimens were reviewed by an experienced pathologist (Dr. Chang LC) and scored by the NAFLD activity score (NAS: steatosis 0-3, lobular inflammation 0-2, hepatocellular ballooning 0-2, and fibrosis 0-4). The diagnosis of NASH was most possible when the NAS score was more than 5 and the diagnosis was not likely when the NAS score was less than 3 [23].
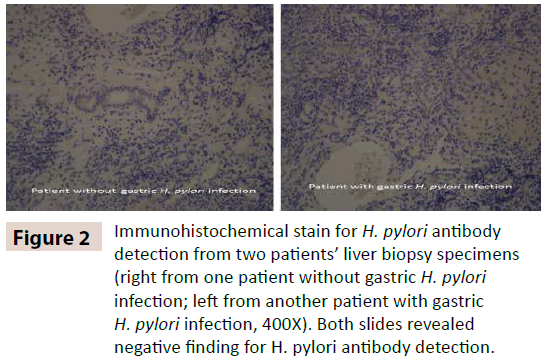
Immunohistochemical stain [IHC] for H. pylori detection
Imunohistochemistry for H. pylori (polyclone, Zytomed Systems GmbH) was performed on formalin-fixed paraffin-embedded tissue from hepatic biopsy specimens. A single representative block from each specimen was sectioned at 3 μm onto positively charged slides. Slides were then stained using the Bond-Max autostainer (Leica Biosystems). Briefly this involved slides being dewaxed in Bond Dewax solution [Leica Biosystems] and hydrated in Bond Wash solution (Leica Biosystems). Antigen retrieval was performed at acidic pH using Epitope Retrieval 1 solution [Leica Biosystems] for 10 min at 100 °C. Slides were then incubated with the primary antibody at a concentration of 1:800 for 30 min at room temperature. The detection kit used was the Bond Polymer Refine Detection kit [DS9800]. The protocol included incubation with post primary antibodies for 8 min, polymerization for 8 min, DAB for 5 min and Haematoxylin for 5 min.
Statistical analysis
The paired-t test was used for comparison of continuous data if the sample size was greater than 30 in each group. However, the Mann-Whitney test was used when the sample size was less than 30. Categorical data were analyzed with the Chi-square test or Fisher’s exact test, where appropriate. All statistical tests were 2-tailed. P<0.05 was considered to represent statistical significance. Statistical analyses were performed using the statistical package SPSS for window [Version 14.0, Chicago, IL, USA].
This research was approved by the Institutional Review Board of the Chang-Gung Memorial Hospital.
Results
Initially 451 patients were enrolled and 44 patients agreed to undergo echo-guided fine needle liver biopsy. Among the 44 patients, NAFLD was diagnosed in 35 patients based on pathologic NAS score and clinical presentation. Six patients were excluded because of taking oral hypoglycemia agents (2 patients) or loss to follow-up (4 patients). Finally, 29 patients (11 patients with H.pylori infection) were included into this study. Demographic data are presented in Table 1. Most patients were centrally obese with waist circumference > 90 cm, had insulin resistance (HOMA-IR value >2.5), body mass index [BMI] ≥ 27 kg/m2 [obesity criteria for Asians] and hypertriglyceridemia (>150 mg/dL). The diagnosis of NASH was made in 10 patients [34.5%, 10/29] with NAS score more than 5. There were no significant differences in age, gender distribution, body weight, and body height or body mass index between the two groups. Laboratory data including fasting plasma glucose, insulin, HOMA-IR, lipid profile, adipokine, inflammatory cytokine, and liver biochemistry and histological findings are presented in Tables 2 and 3. HDL value was the only variable that differed significantly between the two groups. The mean HDL value in patients with H. pylori infection was higher than that in patients without H. pylori infection [50.1 ± 8.8 vs. 38.8 ± 9.7 mg/ dL, p=0.004]. Multivariate linear regression analysis by backward selection revealed waist circumference and triglyceride value, but not H. pylori infection status were the predictors for HOMR-IR value (Table 4). Analysis from the serial values of HOMA-IR from patients 0, 3 or 6 months after eradication therapy revealed no increasing or decreasing trend of HOMA-IR values following H.pylori eradication treatment.
| H. pylori infection N=11 |
No H. pyloriinfection N=18 | P value | |
|---|---|---|---|
| Age | 54.6 ± 11.0 | 49.5 ± 11.3 | 0.24 |
| Gender (F/M) | 4/7 | 3/15 | 0.38 |
| Body height (cm) | 164.2 ± 8.2 | 162.9 ± 8.5 | 0.69 |
| Body weight (Kg) | 72.3 ± 10.3 | 75.2 ± 14.6 | 0.57 |
| BMI† | 26.9 ± 4.2 | 28.2 ± 4.5 | 0.45 |
| Waist circumference (cm) | 93.5 ± 6.9 | 95.1 ± 11.0 | 0.67 |
Table 1 Demographic data.
| H. pylori infection N=11 |
No H. pylori infection N=18 | P value | |
|---|---|---|---|
| Lipid profile | |||
| Cholesterol (mg/dL) | 184.9 ± 50.9 | 181.6 ± 28.9 | 0.83 |
| Triglyceride (mg/dL) | 157.5 ± 84.9 | 155.2 ± 74.4 | 0.94 |
| HDL†(mg/dL)* | 50.1 ± 8.8 | 38.8 ± 9.7 | 0.004 |
| LDL†(mg/dL) | 116.8 ± 23.1 | 113.4 ± 24.7 | 0.71 |
| Adipokine | |||
| Adiponectin(ug/mL) | 6.7 ± 3.4 | 6.6 ± 3.9 | 0.95 |
| Leptin(ng/mL) | 8.2 ± 6.0 | 9.7 ± 5.1 | 0.48 |
| Inflammatory cytokine | |||
| HS-CRP‡(mg/L) | 2.1 ± 1.0 | 1.8 ± 1.8 | 0.61 |
| TNF-α§(pg/mL) | 21.2 ± 23.4 | 17.7 ± 23.8 | 0.70 |
| Blood glucose/insulin | |||
| Fasting glucose (mg/dL) | 113.0 ± 19.9 | 113.0 ± 28.3 | 0.99 |
| Fasting insulin (mU/L) | 12.6 ± 6.5 | 14.6 ± 8.5 | 0.51 |
| HBA1C (%) | 5.9 ± 0.5 | 6.0 ± 0.6 | 0.65 |
| HOMR-IR¶ | 3.4 ± 1.6 | 4.5 ± 3.8 | 0.37 |
‡ High sensitive C-reactive protein
§ Tumor necrosis factor alfa
¶ Homeostasis model assessment of insulin resistance
Table 2 Laboratory data for 29 patients.
| H. pylori infection N=11 |
No H. pylori infection N=18 | P value | |
|---|---|---|---|
| AST (U/L) | 56.5 ± 26.7 | 53.5 ± 40.2 | 0.83 |
| ALT (U/L) | 80.9 ± 45.7 | 63.5 ± 30.6 | 0.23 |
| Alk-P (U/L) | 67.6 ± 17.1 | 76.0 ± 16.3 | 0.71 |
| rGT(U/L) | 59.2 ± 39.6 | 51.1 ± 34.4 | 0.57 |
| Bilirubin (T)(mg/dL) | 1.0 ± 0.4 | 1.1 ± 0.5 | 0.58 |
| Albumin | 4.4 ± 0.4 | 4.5 ± 0.4 | 0.52 |
| Fatty metamorphosis (%) | 53.0 ± 28.0 | 48.0 ± 23.0 | 0.61 |
| Fibrosis score | 1.2 ± 1.2 | 1.0 ± 1.4 | 0.70 |
| NAS† score | 4.7 ± 1.3 | 5.1 ± 1.7 | 0.51 |
Table 3 Liver biochemistry and pathologic studies.
| Factor | Exp(B)† | 95% Confidence Interval(CI) | p value | |
|---|---|---|---|---|
| Waist circumference | 0.206 | 0.080 | 0.332 | 0.003 |
| Triglyceride | 0.014 | 0.001 | 0.027 | 0.036 |
| H. pyloriinfection | -0.849 | -2.897 | 1.198 | 0.398 |
| rGT | 0.009 | -0.003 | 0.021 | 0.126 |
| HR-CRP | -0.849 | -1.703 | 0.005 | 0.051 |
| Leptin | 0.159 | -0.087 | 0.405 | 0.193 |
Table 4 Multivariate linear regression analysis for HOMR-IR value.
The H. pylori eradication success rate in this study was 81.8% [9/11]. For patients with or without gastric H. pylori infection, none of the hepatic specimens showed evidence of H pylori by IHC antibody stain (Figure 2).
Figure 2: Immunohistochemical stain for H. pylori antibody detection from two patients’ liver biopsy specimens (right from one patient without gastric H. pylori infection; left from another patient with gastric H. pylori infection, 400X). Both slides revealed negative finding for H. pylori antibody detection.
Discussion
The hyperinsulinemic-euglycemic clamp technique, the quantitative insulin sensitivity check index [QUICKI] and HOMAIR are all well validated methods for quantitatively assessing IR. Although the hyperinsulinemic-euglycemic clamp technique is considered the gold standard for the assessment of IR, HOMAIR is the most common method for assessment of IR in clinical practice and epidemiologic studies [24,25]. HOMA-IR is a minimally invasive index that requires only fasting serum samples. Although there is no widely accepted normal range for HOMA-IR, the upper cut-off value, which defines IR, has been proposed to be 2.5 [range 2.0 to 3.0] in most studies [18,26,27]. In this study, patients with NASH were included. The mean IR values were 3.4 from patients with H. pylori infection and 4.5 from patients without H. pylori infected group. Hence, the majority of patients in this study demonstrated insulin resistance. Although the data seem to indicate an association between H. pylori infection and IR, it is still unclear whether H. pylori infection plays a role in IR, especially in patients with NASH. It is unknown whether H. pylori triggers IR or whether chronic active H pylori infection promotes IR. We found that HOMA-IR values did not differ significantly between patients with H. pylori infection and those without this infection. Among the patients with H. pylori infection, the serial follow-up HOMA-IR values within the 6-month period following H. pylori eradication treatment didn’t reveal any increasing or decreasing trend. Although some studies have reported an improvement in HOMA-IR following H. pylori eradication, other studies have shown no effect [20,21]. Different follow-up interval and multiple influencing factors of IR most likely contribute to the differences in results from the two studies. H. pylori infection is usually acquired early in life. It has been proposed that H pylori infection might precede H. pylori infection-IR interaction. The original hypothesis was that H. pylori induced chronic gastritis which resulted in IR. Chronic inflammation and alternations in counter-regulatory hormones are deemed responsible for IR pathogenesis. However, the inflammatory cytokine and H. pylori infection status did not reveal reciprocal change during H. pylori eradication treatment in this study. Neither IR nor abnormal ALT improved following H. pylori eradication. Hence, H. pylori eradication may play a minor role in improving IR in patients with NASH.
H. pylori infection can induce dyslipidemia, as it leads to elevated levels of total cholesterol, low-density lipoprotein cholesterol [LDL-C], triglyceride concentrations and decreased levels of highdensity lipoprotein cholesterol [HDL-C] [17,28,29]. Increased HDL has been found in patients with duodenal ulcer following successful H. pylori eradication [28]. However, a higher mean HDL value was seen in patients with H. pylori infection in the current study, which was contrast to the results from some previous studies [17,28,29]. Because there was no statistical difference between the mean values of cholesterol, triglyceride, LDL between patients with H. pylori infection and those without H. pylori infection in this study, the reason of a higher mean HDL value in this study might be resulted from a type I error [small sample size]. Our latter community-based study with a larger sample size (more than 800 subjects) revealed no statistical difference of mean HDL value between subjects with H pylori and those without H pylori infection [30]. However, the result from a community-based study could not imply the same result from a subgroup, such as NAFLD patients. A further study with more NAFLD patients is warrant to elucidate the difference of mean HDL values between patients with and without H pylori infection. A few studies have reported that the 16S recombinant RNA gene of H. pylori was present in liver samples from patients with NASH [31,32]. If there is causality between H. pylori and NASH then H. pylori should be detected in hepatic biopsy specimens from patients with NASH [33]. Failure to detect or culture the bacterium in the liver could be considered an argument against the role of H. pylori in NASH [33]. Other explanations for being unable to detected H pylori by polyclonal antibody stain in this study may be because of low bacterial load and the adaptation of the bacteria to a specific environment, as reported in murine liver [34-36].
In the absence of definitive clinical or laboratory evidence of the above disorders, liver biopsy is the only way to confirm or exclude the diagnosis of NASH. The case number in this study was small because all eligible patients were required to undergo liver biopsy. A further study with a large number of patients is necessary to confirm the difference in HDL value between NAFLD patients with and those without H. pylori.
Conclusion
IR is a common condition in patients with NAFLD. We found that there was no significant difference in HOMA-IR value, adipokine (adiponectin, leptin), inflammatory cytokine [HS-CRP, TNF-α] or liver biochemistry between NAFLD patient with and those without H. pylori infection. The benefit of improving IR was not remarkable following H. pylori eradication for patients with NAFLD and H. pylori infection.
Acknowledgements
This study was supported by CMRPG2A0101 grant.
Ethical Adherence
This research was approved by the Institutional Review Board of the Chang-Gung Memorial Hospital.
References
- Sanyal AJ, Campbell-Sargent C, Mirshahi F, Rizzo WB, Contos MJ, et al. (2001) Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology 120: 1183-1192.
- Chitturi S, Abeygunasekera S, Farrell GC, Holmes-Walker J, Hui JM, et al. (2002) NASH and insulin resistance: Insulin hypersecretion and specific association with the insulin resistance syndrome. Hepatology 35: 373-379.
- Pagano G, Pacini G, Musso G, Gambino R, Mecca F, et al. (2002) Nonalcoholic steatohepatitis, insulin resistance, and metabolic syndrome: further evidence for an etiologic association. Hepatology 35: 367-372.
- Marchesini G, Brizi M, Morselli-Labate AM, Bianchi G, Bugianesi E, et al. (1999) Association of nonalcoholic fatty liver disease with insulin resistance. Am J Med 107: 450-455.
- Musso G, Gambino R, Durazzo M, Biroli G, Carello M, et al. (2005) Adipokines in NASH: postprandial lipid metabolism as a link between adiponectin and liver disease. Hepatology 42: 1175-1183.
- Cohen B, Novick D, Rubinstein M (1996) Modulation of insulin activities by leptin. Science 274: 1185-1188.
- Marchesini G, Pagotto U, Bugianesi E, De Iasio R, Manini R, et al. (2003) Low ghrelin concentrations in nonalcoholic fatty liver disease are related to insulin resistance. J ClinEndocrinolMetab 88: 5674-5679.
- Angulo P (2002) Nonalcoholic fatty liver disease. N Engl J Med 346: 1221-1231.
- Pappo I, Bercovier H, Berry E, Gallilly R, Feigin E et al. Antitumor necrosis factor antibodies reduce hepatic steatosis during total parenteral nutrition and bowel rest in the rat. J Parenter Enteral Nutr 19: 80-82.
- Kirsch R, Clarkson V, Verdonk RC, Marais AD, Shephard EG et al. (2006) Rodent nutritional model of steatohepatitis: effects of endotoxin [lipopolysaccharide] and tumor necrosis factor alpha deficiency. J Gastroenterol Hepatol 21: 174-182.
- Abu-Shanab A, Quigley EM (2010) The role of the gut microbiota in nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol 7: 691-701.
- Peach HG, Barnett NE (2001) Helicobacter pylori infection and fasting plasma glucose concentration. J ClinPathol 54: 466-469.
- Aydemir S, Bayraktaroglu T, Sert M, Sokmen C, Atmaca H, et al. (2005) The effect of Helicobacter pylori on insulin resistance. Dig Dis Sci 50: 2090-2093.
- Roper J, Francois F, Shue PL, Mourad MS, Pei Z, et al. (2008) Leptin and ghrelin in relation to Helicobacter pylori status in adult males. J Clin Endocrinol Metab 93: 2350-2357.
- Azuma T, Suto H, Ito Y, Ohtani M, Dojo M, et al. (2001) Gastric leptin and Helicobacter pylori infection. Gut 49: 324-329.
- Candelli M, Rigante D, Marietti G, Nista EC, Crea F, et al. (2003) Helicobacter pylori, gastrointestinal symptoms, and metabolic control in young type 1 diabetes mellitus patients. Pediatrics 111: 800-803.
- Gunji T, Matsuhashi N, Sato H, Fujibayashi K, Okumura M, et al. (2008) Helicobacter pylori infection is significantly associated with metabolic syndrome in the Japanese population. Am J Gastroenterol 103: 3005-3010.
- Gunji T, Matsuhashi N, Sato H,Fujibayashi K, Okumura M et al. (2009) Helicobacter pylori infection significantly increase insulin resistance in the asymptomatic Japanese population. Helicobacter 14:144-150.
- Polyzos SA, Kountouras J, Zavos C, Deretzi G (2011) The association between Helicobacter pylori infection and insulin resistance: a systematic review. Helicobacter 16: 79-88.
- Gen R, Demir M, Ataseven H (2010) Effect of Helicobacter pylori eradication on insulin resistance, serum lipids and low-grade inflammation. South Med J 103: 190-196.
- Park SH, Jeon WK, Kim SH, Kim HJ, Park DI, et al. (2005) Helicobacter pylori eradication has no effect on metabolic and inflammatory parameters. J Natl Med Assoc 97: 508-513.
- Matthews DR, Hosker JP, Rudenski AS,Naylor BA, Treacher DF, et al. (1985) Homeostasis model assessment: insulin-resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412-419.
- Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, et al. (2005) Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41: 1313-1321.
- Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, et al. (200) Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care 23:57-63.
- Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27: 1487-1495.
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, et al. (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia28:412-419.
- Tresaco B, Bueno G, Pineda I, Moreno LA, Garagorri JM, et al. (2005) Homeostatic model assessment (HOMA) index cut-off values to identify the metabolic syndrome in children. J PhysiolBiochem 61: 381-388.
- Scharnagl H, Kist M, Grawitz AB, Koenig W, Wieland H, et al. (2004) Effect of Helicobacter pylori eradication on high-density lipoprotein cholesterol. Am J Cardiol 93: 219-220.
- Kamada T, Hata J, Kusunoki H, Ito M, Tanaka S, et al. (2005) Eradication of Helicobacter pylori increases the incidence of hyperlipidaemia and obesity in peptic ulcer patients. Dig Liver Dis 37: 39-43.
- Chen LW, Chien CY, Yang KJ, Sheng-Fong Kuo, Chih-Hung Chen, et al. Helicobacter pylori Infection Increases Insulin Resistance and Metabolic Syndrome in Residents Younger than 50 Years Old: A Community-Based Study.
- Cindoruk M, Cirak MY, Unal S, Karakan T, Erkan G, et al. (2008) Identification of Helicobacter species by 16S rDNA PCR and sequence analysis in human liver samples from patients with various etiologies of benign liver diseases. Eur J GastroenterolHepatol 20: 33-36.
- Pirouz T, Zounubi L, Keivani H, Rakhshani N, Hormazdi M (2009) Detection of Helicobacter pylori in paraffin-embedded specimens from patients with chronic liver diseases, using the amplification method. Dig Dis Sci 54: 1456-1459.
- Hill AB (1965) THE ENVIRONMENT AND DISEASE: ASSOCIATION OR CAUSATION? Proc R Soc Med 58: 295-300.
- Pellicano R, Ménard A, Rizzetto M, Mégraud F (2008) Helicobacter species and liver diseases: association or causation? Lancet Infect Dis 8: 254-260.
- Avenaud P, Marais A, Monteiro L, Le Bail B, Bioulac Sage P, et al. (2000) Detection of Helicobacter species in the liver of patients with and without primary liver carcinoma. Cancer 89: 1431-1439.
- Fox JG, Li X, Yan L, Cahill RJ, Hurley R, et al. (1996) Chronic proliferative hepatitis in A/JCr mice associated with persistent Helicobacter hepaticus infection: a model of helicobacter-induced carcinogenesis. Infect Immun 64: 1548-1558.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences